Surveiller l’utilisation des connaissances
Index
Après le déploiement des interventions de mise en œuvre, les équipes de changement doivent déterminer si le changement de pratique et toutes ses composantes ont été réalisés et, par conséquent, si les interventions mises en œuvre pour soutenir ce ou ces changements ont été efficaces. Pour en savoir plus, consultez cette section consacrée à la phase « Suivi de l'utilisation des connaissances » du cycle d'action du KTA.
Quelle est cette phase ?
Assurer le suivi de l’utilisation des connaissances
Qu’est-ce que la phase « assurer le suivi de l’utilisation des connaissances »?
Une fois la nouvelle intervention ou pratique mise en œuvre dans votre contexte local, il faut en surveiller l’adoption au fil du temps (AIIAO, 2002; Graham et coll., 2006). Le suivi comprend le processus continu de collecte et d’analyse de données afin de comparer la mise en œuvre d’une intervention ou d’une pratique avec les objectifs prévus. Il comprend la collecte, l’examen et l’analyse systématiques des données. Les sources de données peuvent comprendre des notes d’évolution, des bases de données cliniques, des entrevues auprès de professionnels de la santé qui participent au changement de pratique, des questionnaires ou d’autres indicateurs de données qui fourniront l’information pertinente.
Le suivi de l’utilisation des connaissances répond aux questions suivantes :
- Les activités sont-elles mises en œuvre comme prévu?
- Les connaissances, la pratique ou l’intervention sont-elles utilisées?
- Les connaissances, les attitudes et les croyances des utilisateurs cibles sont-elles modifiées en raison de ces nouvelles connaissances, pratiques ou interventions?
Suivi de la mise en œuvre et de l’adoption des interventions et des programmes
Votre unité ou organisation peut mettre en œuvre une intervention ou un programme complets, ainsi que des informations visant à changer les attitudes et les comportements des intervenants (utilisation conceptuelle), la pratique clinique (utilisation instrumentale) ou la politique (utilisation persuasive) (Strauss et coll., 2013).
Le suivi de l’adoption des interventions et des programmes est essentiel pour comprendre si les ressources allouées à la mise en œuvre de ces interventions et programmes en valent la peine, ce qui vous permet en fin de compte d’atteindre votre objectif souhaité de changer les résultats cliniques.
Utilisation d’indicateurs de processus pour le suivi de la mise en œuvre
Les indicateurs de processus suivent les progrès de l’intervention ou du changement de pratique mis en œuvre. Ils aident à répondre à la question suivante : « Les activités sont-elles mises en œuvre comme prévu? » Voici quelques exemples d’indicateurs de processus :
- le nombre de séances de formation tenues pour les professionnels de la santé
- le nombre d’activités de sensibilisation menées par l’équipe de changement
- le pourcentage de professionnels de la santé joints à l’aide de messages clés sur les interventions ou la pratique
Pourquoi la phase « assurer le suivi de l’utilisation des connaissances » est-elle importante?
Le suivi de l’utilisation des connaissances est important, parce que cette phase détermine comment, et dans quelle mesure, les utilisateurs cibles tels que le personnel au point d’intervention utilisent la pratique ou les connaissances (AIIAO, 2012; Strauss et coll., 2013).
Le suivi de l’utilisation des connaissances montre dans quelle mesure :
- les connaissances sont communiquées aux utilisateurs ciblés qui doivent en être informés ou les utiliser
- les recommandations des LDPE sélectionnées sont connues, acceptées et appliquées
- l’intervention ou la pratique est utilisée correctement
Évaluation de l’utilisation des connaissances
L’utilisation des connaissances est un aspect essentiel de l’adhésion des fournisseurs aux pratiques fondées sur les données probantes et aux recommandations. Elle peut :
- changer les attitudes et les croyances à l’égard d’une pratique donnée (par exemple, un professionnel de la santé se renseigne sur une pratique exemplaire, développe des attitudes positives à son égard et acquiert la motivation de l’appliquer)
- être complexe (les professionnels de la santé peuvent choisir de suivre certaines recommandations, mais pas d’autres)
- être influencée par les structures et les processus dans l’établissement clinique
Types d’utilisation des connaissances
Les agents de changement devraient tenir compte de trois principaux types d’utilisation des connaissances lorsqu’ils la mesurent (Strauss et coll., 2013) :
|
Type d’utilisation des connaissances |
Définition |
Exemple |
Dimensions à mesurer |
Exemples de suivi de l’utilisation des connaissances |
|
|
Conceptuelle |
Compréhension et intériorisation des nouvelles connaissances. Les résultats indiquent des changements dans les connaissances, la compréhension ou les attitudes à l’égard d’une pratique ou d’une intervention |
L’utilisation de recensions des écrits, d’études évaluées par des pairs et de documents d’orientation peut changer la façon de penser et éclairer la prise de décisions sans modifier directement les pratiques |
Attitude Niveau de connaissances Croyances Intérêt Autoefficacité |
Faire une vérification des connaissances avant et après une séance d’enseignement sur l’hygiène des mains afin de déterminer la compréhension des participants |
|
|
Instrumentale |
Application concrète des connaissances Décrit les changements de comportement ou de pratique et de connaissances lorsqu’ils sont traduits sous une forme utilisable |
Utilisation d’aides à la décision, d’une nouvelle intervention ou d’une nouvelle pratique |
Utilisation de la recherche Acceptabilité Faisabilité Adoption Indicateurs de fidélité |
Effectuer un audit des dossiers afin de déterminer si les recommandations des LDPE sont suivies
Observer la pratique en temps réel |
|
|
Les connaissances sont utilisées comme un outil de persuasion. Il s’agit de l’utilisation des connaissances pour obtenir un pouvoir particulier ou pour influer sur les résultats ou les objectifs (par exemple, un changement de politique) |
Inclure les résultats d’un sondage sur la satisfaction des patients qui a indiqué que les patients étaient insatisfaits de la gestion de leur besoin de soulagement de la douleur, pour aider les praticiens à adopter les recommandations de la LDPE sur la douleur |
Changement de politique |
Interroger les praticiens pour savoir s’il y a eu un changement dans les politiques concernant une pratique particulière dans le milieu de travail |
Méthodes de collecte de données pour assurer le suivi de l’utilisation des connaissances
Envisagez d’utiliser les méthodes de collecte de données suivantes pour assurer le suivi de l’utilisation des connaissances par les professionnels de la santé ou de l’adoption de l’intervention ou de la pratique.
- Audit et rétroaction : Vous pouvez recueillir des données sur certains aspects précis de la nouvelle intervention ou pratique, les résumer et fournir aux fournisseurs de soins de santé les résultats sur la façon dont ils peuvent s’améliorer (Colquhoun et coll., 2017; AIIAO, 2012).
- Groupe de discussion : Vous pouvez animer une discussion au sein d’un groupe d’intervenants au sujet des expériences, attitudes ou comportement des membres du groupe à l’égard de l’intervention ou de la pratique. Les groupes de discussion offrent des interactions dynamiques en groupe en réponse à vos questions d’orientation. Ces interactions de groupe peuvent fournir des informations utiles sur le déroulement du changement de pratique ou de la nouvelle intervention.
- Entrevues : Vous pouvez mener des entrevues approfondies et en tête-à-tête pour interroger les intervenants sur leurs expériences, leurs attitudes ou leurs comportements à l’égard de l’intervention ou du changement de pratique (AIIAO, 2012).
- Observation : Vous pouvez effectuer des observations pendant les réunions matinales, les réunions d’équipe et la pratique clinique, qui peuvent vous aider à comprendre si le changement a été mis en œuvre dans votre milieu (AIIAO, 2012).
- Sondages : Vous pouvez demander aux intervenants de remplir des questionnaires structurés assortis d’échelles de notation. Vous pouvez également inclure des questions ouvertes. Les sondages peuvent se faire en personne, par téléphone ou par Internet (Dillman, 2007).
Si le niveau d’utilisation des connaissances et d’adoption de la pratique est acceptable, vous pourriez commencer à envisager des stratégies de suivi au cours de la phase de durabilité. Les entrevues auprès des intervenants peuvent être utiles pour déterminer les méthodes qui pourraient être les plus efficaces.
Si le niveau d’utilisation des connaissances ou d’adoption de la pratique est inférieur aux attentes ou au niveau souhaité, il peut être utile de réévaluer les obstacles à l’utilisation des connaissances ou de modifier les stratégies de mise en œuvre en conséquence.
Déterminer les rôles, les responsabilités et les échéanciers du suivi
- Attribuez la responsabilité de la collecte des données afin que chacun soit au fait de ses rôles et responsabilités. Cela permet également aux nouveaux membres de l’équipe de changement de se joindre au projet et de se faire une idée de qui est responsable de quoi, de ce dont ils peuvent être responsables et quand.
- REMARQUE : La collecte des données de suivi peut se faire régulièrement à des intervalles courts ou plus longs. Selon l’intervention ou la pratique, il peut s’agir d’une collecte hebdomadaire, mensuelle, trimestrielle, semestrielle ou annuelle.
- Notez toutes les exigences nécessaires à la collecte des données, comme la dotation en personnel et les fonds. Assurez-vous d’inclure des activités de suivi dans votre budget (fonds, ressources humaines, équipement).
SOURCE : Evaluation Toolbox, 2010
Accélérez votre succès : Lorsque vous assurez le suivi de l’adoption de l’intervention ou de la pratique, vous et votre équipe voudrez peut-être prêter attention à tout « leader émergent ». Les leaders émergents sont les premiers adeptes au changement; ils peuvent être des modèles de rôle dans l’application de la pratique ou de l’intervention dans leur travail. Consultez l’aspect « leaders émergents » du cadre d’action du mouvement social pour apprendre comment reconnaître les leaders émergents qui soutiennent le changement. Vous voudrez peut-être trouver des moyens de les soutenir afin qu’ils deviennent des agents de changement pour votre projet de changement!
Importance de l’évaluation des connaissances, des attitudes et des croyances
- Les connaissances, attitudes et croyances des fournisseurs au sujet de la nouvelle pratique ou intervention peuvent jouer un rôle crucial dans la mesure dans laquelle ils utilisent la pratique ou l’intervention (Cook et coll., 2015).
- Les perceptions des fournisseurs à l’égard d’une intervention peuvent constituer un obstacle ou un élément facilitateur pour sa mise en œuvre (Aarons, 2006; Henggeler et coll., 2008; Jensen-Doss et coll., 2009).
- Les connaissances, les attitudes et les croyances des fournisseurs peuvent influer sur :
- leur volonté de faire l’essai de la nouvelle pratique ou de l’intervention
- la façon dont ils présentent toute nouvelle activité aux personnes
- leur volonté de poursuivre une nouvelle pratique en cas de difficultés (Cook et coll., 2015)
Pourquoi mesurer les connaissances, les attitudes et les croyances dans le cadre du suivi de l’utilisation des connaissances?
- L’adoption d’une nouvelle pratique ou d’une intervention est étroitement liée aux connaissances et à l’attitude des professionnels de la santé.
- Le fait de reconnaître que les professionnels de la santé estiment peut-être que la nouvelle pratique ou l’intervention est incompatible avec leurs pratiques existantes, ou manifestent une résistance quelconque, peut vous permettre de résoudre ces problèmes dès le départ (Cook et coll., 2015).
- L’obtention de mesures validées et fiables des connaissances, des attitudes et des croyances des professionnels de la santé à l’égard de la nouvelle pratique ou de l’intervention peut donner un aperçu de la façon dont ils la comprennent et la perçoivent.
Le tableau ci-dessous présente des exemples de mesures des connaissances, des attitudes et des comportements, ainsi que les résultats correspondants qui représentent l’utilisation des connaissances.
|
Type de résultat |
Façons de documenter le résultat |
Moment où le résultat est susceptible d’être évident |
|
Connaissances changées |
|
|
|
Attitudes alignées sur les connaissances |
|
|
|
Comportement aligné sur les connaissances |
|
|
SOURCES : AIIAO, 2012; The Improve Group, 2010.
Pourquoi cette phase est-elle importante ?
Le suivi de l'utilisation des connaissances est important, car cette phase détermine comment et dans quelle mesure la pratique ou les connaissances sont utilisées par les utilisateurs cibles, comme le personnel des points de service (RNAO, 2012 ; Strauss et al., 2013).
Le suivi de l'utilisation des connaissances montre dans quelle mesure :
les connaissances sont communiquées aux utilisateurs cibles qui doivent en être informés ou les utiliser ;
les recommandations des lignes directrices sur les meilleures pratiques sélectionnées sont connues, acceptées et appliquées ; et
l'intervention ou la pratique est utilisée correctement.
Case study

Leveraging innovative quality monitoring - Humber River Hospital
A major acute-care hospital in Toronto, Ontario, Humber River Hospital (now Humber River Health) has used continuous monitoring to determine the impact of their BPG implementation and staff performance.
These tiles, displayed on large screen monitors in a Command Centre (pictured above), are integrated into the daily delivery of care to support physicians, nurses, and other clinical staff. Each row within the tile represents a patient, followed by where they are located. By clicking on a patient, staff can see more information regarding the clinical criteria that put them on the tile.
With every patient, there is an expected time in which the issue should be resolved based on a service level set by the hospital. If the system detects that the process is taking longer than expected, the icon will escalate to amber and then to red, indicating a higher level of alert.
Tiles also include several quality monitoring indicators based on RNAO's best practice guidelines (BPG) related to fall risk intervention, wound and skin management, pain management and delirium management. By centralizing data in the Command Centre, the monitoring indicators empower clinicians so that they can intervene in a timely manner to ensure that best practices are followed.
Read more about this innovative quality monitoring approach here: https://www.hrh.ca/2020/08/04/cc-risk-of-harm/
Conseils pratiques
- Déterminez le niveau minimum acceptable d’utilisation ou d’adoption des connaissances par le personnel pour les nouvelles pratiques ou les interventions. Par exemple, quel serait, selon vous, le niveau minimal de connaissances que les professionnels de la santé doivent acquérir pour procéder à un changement de pratique?
- Établissez les indicateurs clés qui permettront à votre équipe de déterminer que le niveau minimum acceptable est atteint.
- Réfléchissez à l’incidence de ce niveau minimum acceptable sur les résultats que vous avez entrepris d’atteindre en lançant une nouvelle pratique ou une intervention.
- Obtenez un plan de mesure de l’utilisation des connaissances ou de l’adoption de l’intervention ou de la pratique à l’aide d’au moins l’une des méthodes de cette section (par exemple, audit et rétroaction, observation, ou sondages).
- Déterminez la fréquence et les périodes appropriées pour ces mesures.
- Utilisez des mesures validées et fiables, dans la mesure du possible.
KTA Tools

Applying pragmatic and valid tools can support change teams to accurately monitor knowledge use and strengthen their understanding of these factors. Looking at the results of using the tool can also help change teams prepare for the next action cycle phase, “Evaluate outcomes”.
For each tool, two documents are provided
- a summary page that includes the tool’s purpose, description and applicable action cycle phases
- a companion document that details the tools’ pragmatic and psychometric properties.
NOTE:
*All of the tools listed can also be considered for use during the action cycle phase: Assess barriers and facilitators to knowledge use.
**All of the tools listed can be considered for use during the action cycle phases: Identify the problem/Determine the know/do gap and Assess barriers and facilitators to knowledge use.
Valid KTA Tools
Vérifiez vos progrès
- vous avez prévu de surveiller différents types de connaissances
- vous avez reçu une rétroaction de votre équipe ou de vos pairs sur la pertinence des méthodes que vous avez suggérées pour mesurer l’utilisation des connaissances ou l’adoption d’une nouvelle pratique
- vous avez déterminé les outils que vous pouvez utiliser pour mesurer l’utilisation des connaissances
Lien entre cette phase et les autres volets du cadre de référence
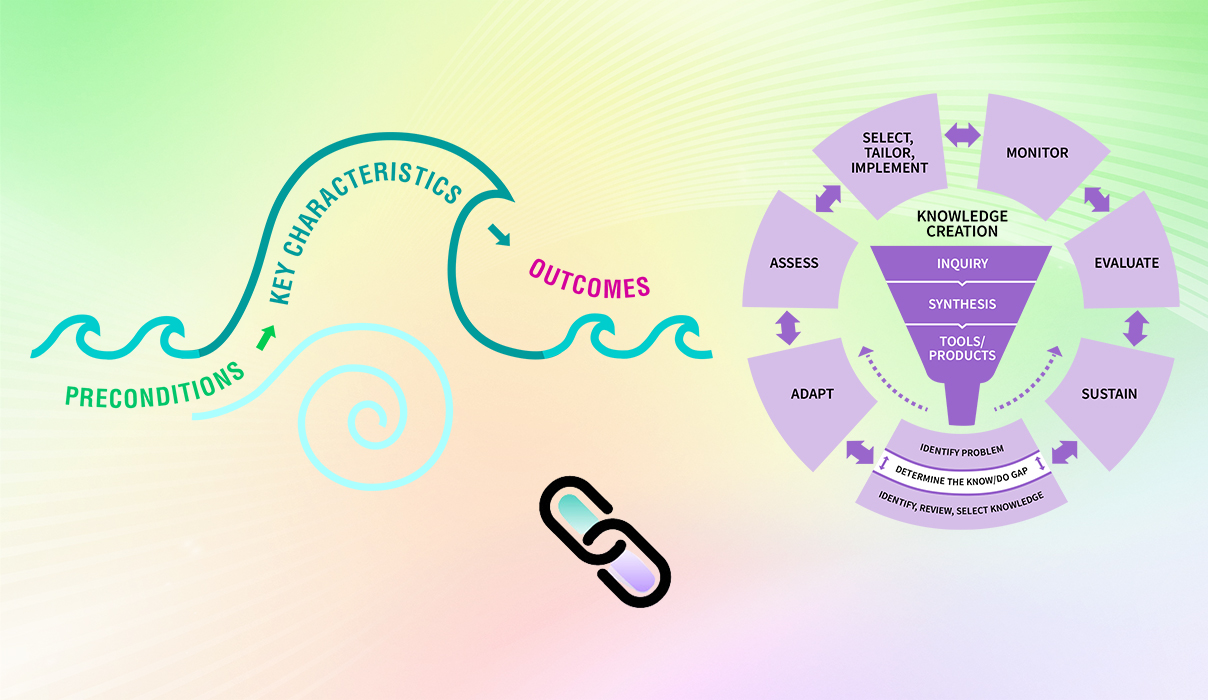
Lien entre cette phase et les éléments du cadre d’action du mouvement social :
Vous pouvez renforcer ou accélérer votre capacité et celle de votre équipe de changement dans la phase « assurer le suivi de l’utilisation des connaissances » en ajoutant certains éléments du cadre d’action du mouvement social (AMS), car les deux cadres de référence sont complémentaires et utilisés conjointement pour accélérer l’adoption et la durabilité du changement. En plus de l’exemple de lien décrit précédemment dans cette section, il peut y avoir de nombreux autres points de liaison entre les deux cadres. Vous trouverez ci-dessous deux exemples à prendre en considération :
- Motivation intrinsèque :Vous et votre équipe de changement pouvez considérer la motivation intrinsèque comme un facteur qui contribue positivement à l’utilisation des données probantes dans leurs milieux locaux. La motivation intrinsèque peut s’évaluer en fonction des connaissances, des attitudes et des croyances des gens au sujet du changement. Plus le personnel est intrinsèquement motivé, plus il est susceptible d’adhérer au changement.
- Leadership émergent : Le leadership émergent, qu’il soit officiel ou officieux, suit une progression naturelle au sein de l’équipe et peut mener au suivi de l’utilisation des connaissances. Les leaders émergents jouent le rôle de modèles influents et de courtiers du savoir qui peuvent avoir une incidence positive sur les connaissances, les attitudes et les croyances à l’égard du changement et de l’adhésion au changement.
Pour en savoir plus sur les liens dynamiques entre les éléments du cadre d’AMS et du cadre d’AC, consultez la section « Accélérez votre succès grâce à la Boîte à outils de la conduite du changement ».
Préparation en vue de la phase suivante : Une fois que vous avez assuré le suivi des connaissances, des attitudes et des comportements des intervenants à l’égard du changement de pratique, vous êtes prêt à évaluer les résultats du changement de pratique. Vous et votre équipe répondrez à des questions telles que « Quelle est l’incidence du changement sur la pratique clinique? » et « Comment le changement a-t-il influé sur les résultats chez les patients et d’autres résultats connexes? »