Select, tailor and implement interventions
Index
Making change often requires multiple approaches (or implementation interventions) to address the assessed barriers and facilitators (as discussed in the previous section of the KTA Framework). Learn more about these strategies in the section below.
What is this phase?
Once barriers and facilitators to knowledge use are identified, you are ready to select, tailor and implement the practice change in your setting. To effectively implement the practice change in your setting, you must use effective implementation strategies. Through careful planning, you can use these strategies to address the barriers you identified in the previous action cycle phase.
This phase requires careful planning – helps you select the right strategies, and tailor them to your local context.
Implementation strategies
Implementation strategies are methods or techniques used to enhance the uptake, implementation, and sustainability of an intervention, program, or practice (Proctor et al., 2013). There is a huge range of strategies, addressing different scales, intended outcomes, settings into which they are applied and the nature of the practice change or interventions to be supported. For example, the Expert Recommendations for Implementing Change (ERIC) taxonomy (Powell et al., 2015) has 73 implementation strategies and the Behaviour Change taxonomy has 93 strategies (Michie et al., 2013) for health-care settings that vary in their impact and feasibility (Powell et al., 2015; Waltz et al., 2015).
Here are some examples of implementation strategies from the ERIC taxonomy (Powell et al., 2015):
- capture and share local knowledge
- conduct educational outreach visits to inform others about the innovation
- identify and prepare champions
- inform local opinion leaders about the innovation
- develop a formal implementation plan
- distribute educational materials
- provide clinical supervision
- remind clinicians
To access the paper that outlines the ERIC taxonomy, look for the “More resources” section below.
Why is this phase important?
Tailored implementation strategies are more likely to support implementation efforts. Contextual factors can influence implementation outcomes through their effects on the ways that support systems or delivery systems enact strategies or how strategies function (Leeman and Nilsen, 2020).
Two examples:
- Staffing shortages in a busy intensive care unit may affect the staff's ability to fully engage in implementation processes, resulting in low use of the new intervention.
- Implementation processes may need to be refined to involve less frequent and/or shorter meetings.
- Staffing shortages may also limit the number of staff that the unit sends to a learning collaborative.
- The learning collaborative may need to be converted to a blended format that combines one brief in-person meeting with a series of conference calls.
Positive change is more likely to occur if you take the time needed to plan effective implementation. Unfortunately, many strategies are implemented without a planned process – they are often chosen based on “common sense” or what has worked in another organization (Michie, 2011).
Consider reviewing a range of strategies and planning and using a process to identify those most likely to be effective (Michie 2011). For example, you can use a planned approach to select strategies that address barriers and leverage facilitators in your local setting.
Avoid the “ISLAGIATT” principle* (It Seemed Like A Good Idea at the Time)
*Coined by Marin Eccles, implementation researcher, for implementing change.
Case study

Implementing effective interventions for drug and alcohol use using Screening, Brief Intervention and Referral to Treatment (SBIRT)
Screening, Brief Intervention, and Referral to Treatment (SBIRT) is endorsed by the Substance Abuse and Mental Health Services Administration as an effective intervention for drug and alcohol use. SBIRT has been implemented in multiple health-care settings including acute care.
Implementation leaders were asked to identify barriers, facilitators, as well as implementation strategies that would be most helpful. From this review, implementation leaders perceived that providing ongoing consultation to clinicians for using SBIRT, distributing educational materials to clinicians, and conducting audits and providing feedback were the most helpful.
All implementation leaders voiced the value of available training resources, and peer support as they moved through the implementation process.
Implementation leaders felt more confident leading change in the future due to the knowledge and skills they developed during SBIRT implementation. They also learned the importance of leveraging support from other interprofessional team members, such as social workers and clinical educators.
Read more about it here. Learn more about SBIRT here. Or, review our best practice guideline, Engaging Clients Who Use Substances.
Practice tips
-
Select and tailor implementation strategies based on the practice barriers you want to address in your context.
-
Choose implementation strategies that can be used in combination or independently, depending on your objectives and your context. No single strategy is effective in all contexts/settings – there is no “one size fits all”. In some cases, it may be more effective to use a single strategy and focus on one key problem of implementation instead of trying to tackle numerous problems using complex, multifaceted strategies. (Lau et al., 2015; Squires et al., 2014)
- Using more strategies at the same time does not always lead to higher chances of implementation success (Wuchner et al., 2014).
- The complexity of strategies may dilute the key benefits of the practice change and reduce the ability of health professionals to understand or acquire the information they need to change practice (LaRocca et al., 2015).
- Use simple or single implementation strategies as they can be as effective as multiple interventions, or interventions with multiple parts.
-
Engage various staff and others to help determine who can help you identify the barriers in your setting.
-
Identify strategies early in the change process.
- Prioritize the strategies that can both address potential barriers and are feasible to implement.
The table below displays a list of features of effective and ineffective strategies (LaRocca et al., 2012; Lau et al., 2015; Squires et al., 2012; Yost et al., 2015).
|
Image

|
Features of effective strategies:
|
|
Image

|
Features of ineffective strategies:
|
Methods to select and tailor strategies
We outline three approaches to select and tailor strategies in the table below, that we’ve taken from the literature. We will then describe intervention mapping and concept mapping in more detail.
Main approaches to select and tailor strategies
|
Name of resource and source |
Brief description |
Advantages |
Disadvantages |
|
Concept mapping |
Involves generating, structuring, and analyzing ideas to create a visual map of concepts that are rated on specified dimensions (e.g., importance and feasibility).
**Note: an adapted method of concept mapping can provide a pragmatic approach to select and tailor implementation strategies to your setting through stakeholder perspectives. |
A participatory process that builds engagement in stakeholders. The ratings allow for the identification of barriers that may be most important and feasibly addressed. |
May require further training or methodological consultation. |
|
A systematic, multi-step method for developing implementation strategies that incorporate theory, evidence, and stakeholder perspectives.
** Note: Intervention mapping is primarily used by researchers, but would require incorporating at least one theory or framework to develop or select your strategies. |
Provides a systematic way of operationalizing the strategy development process. Explicitly incorporates theory, evidence, and stakeholder perspectives. |
May require further training or methodological consultation to incorporate theory, evidence and stakeholder perspectives. |
|
|
Requires staff and others to select different “strategy profiles”, which allows for the determination of how they value different attributes of services, interventions, implementation strategies, etc. |
Provides a clear step-by-step method for selecting and tailoring strategies to unique settings. Forces staff and others to consider attributes of strategies at a granular level, enhancing the precision with which strategies are tailored to the context. |
May yield what staff and others desire, but not what is actually feasible. |
SOURCE: Table adapted from Powell et al., 2017.
Looking in-depth: Steps to intervention mapping and concept mapping
Promoting a practice change to persons and families
- Sometimes, you might want to promote a new practice or a new intervention to persons with lived experience. There are many strategies that can be used to engage this group of individuals. Broadly, the Health System Evidence Taxonomy broadly classifies person-centred strategies into six categories (Chapman et al., 2020):
- Information or education provision: strategies to enable consumers to know about their treatment and their health.
- Behaviour change support: interventions that focus on the adoption or promotion of health and treatment behaviors at an individual level, such as adherence to medicines.
- Skills and competencies development: strategies that focus on the acquisition of skills relevant to self-management.
- (Personal) support: interventions that provide assistance and encouragement to help patients cope with and manage their health and ongoing medical issues, such as counseling and follow-up on treatment efficacy.
- Communication and decision-making facilitation: strategies to involve consumers in decision-making about health care.
- System participation: interventions to involve patients and caregivers in decision-making processes at a system level.
Check your progress
- You engaged key staff and others to help you decide which strategies to use and how they can be tailored to your context.
- You identified implementation strategies that you can use to help with implementing your practice change.
- You have a plan on how to implement each strategy (for example, when should the strategy be implemented? Who will be involved?).
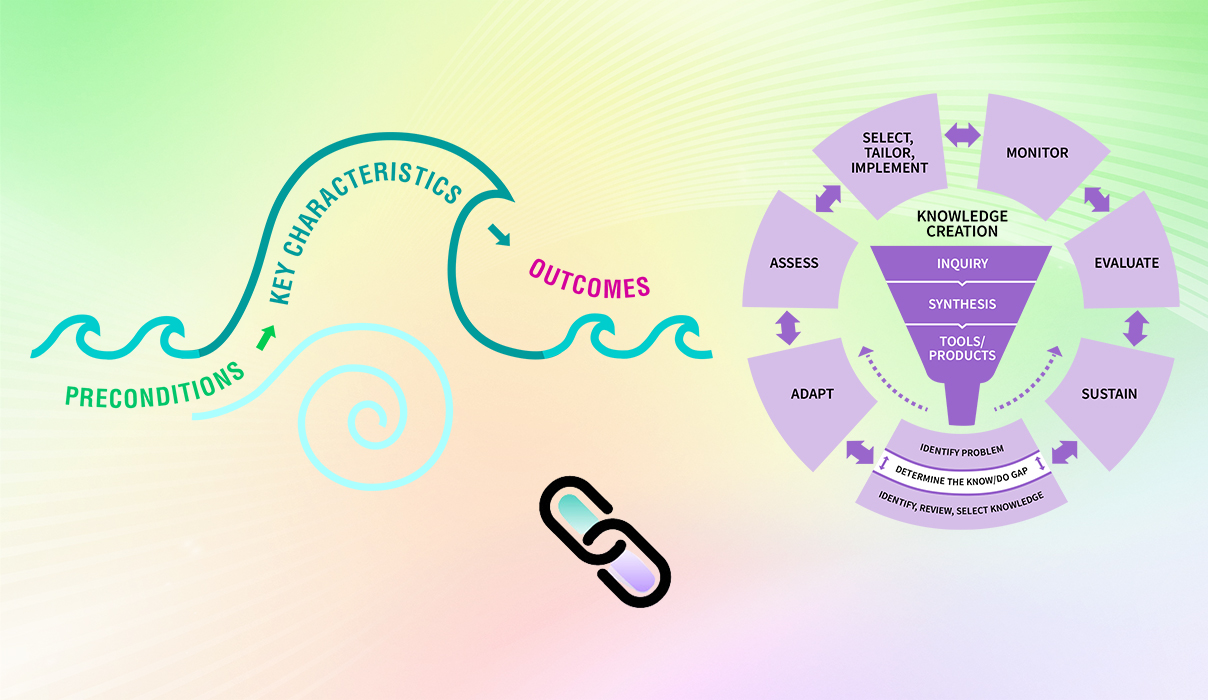
Linking this phase to the elements of the Social Movement Action Framework
You and your change team’s capacity in the “Select, tailor and implement interventions” phase may be enhanced or accelerated by adding in some of the elements of the Social Movement Action (SMA) Framework, as the two frameworks are complementary. There can be many other points of connection between the two frameworks. Below are three examples for you to consider:
- Social movements and their exemplars are visible: By understanding social movements, their exemplars and strategies; you and your change team may identify strategies that were used in social movements that can also be applied to this KTA phase. For example, mobilizing individual and collective action involves people coming together to collaborate for a shared purpose. Applying social movement thinking and their exemplars to selected, tailored and implementation interventions may strengthen the approach to change.
- Public visibility: One key component of the social movement action framework is to increase public visibility of individual and collective actions. You and your change team can use public visibility as a strategy to spotlight your practice change. Public visibility, such as using social media increases awareness, adds credibility to the change and supports the building of a critical mass of supporters and others engaged in the change (Serna-Restrepo, et al 2018).
- Momentum: You and your change team may consider engaging key partners to build momentum when you mobilize your practice change. Momentum – a key component in social movements – is created through strategic planning by a group of people who are actively engaged in the change. Momentum acts as a force of energy that fuels change – in contrast when momentum is absent, the lack of energy surrounding the change may negatively impact the uptake of the practice (Serna-Restrepo, et al, 2018).
For more discussion about the dynamic links between the elements of the SMA Framework to the KTA Framework, see the section "Two complementary frameworks".
Getting ready for the next phase: Once you implemented the practice change in your setting, the next phase is to monitor the uptake of this practice. Are the providers using this practice? Have providers' knowledge, attitudes and beliefs changed as a result of the new practice or knowledge? What is the degree to which the intervention is delivered according to the original design and plan? These are important questions to answer when you have implemented a practice change in your setting.
More resources
Want to learn more about using the strategies of the SMA and KTA frameworks to support your change? Sign up for the RNAO Best Practice Champions training course.