Identify the problem
Index
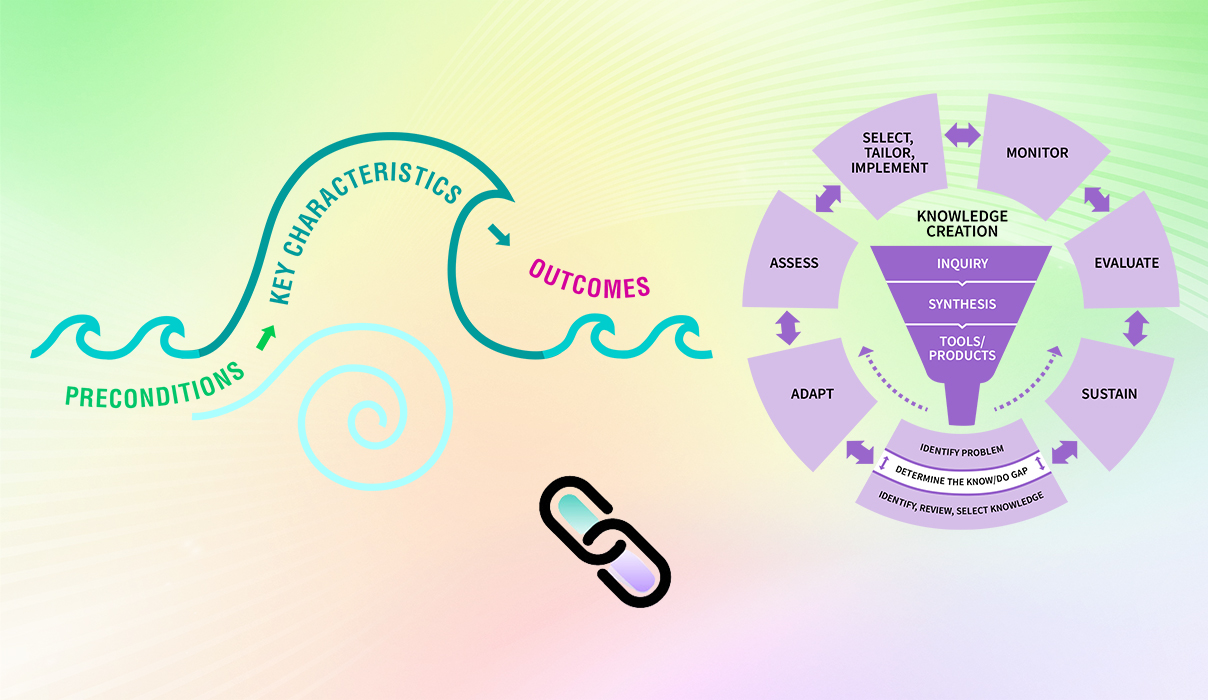
Any change process needs a starting point to focus work and support getting started with planning. Learn more below about the "Identify the problem" phase that helps change teams and others to determine:
- an identified (and prioritized) problem or opportunity for change,
- the extent of the know-do gap (that is, the difference between current practice and best practices), and
- a suitable knowledge tool (e.g., a best practice guideline) that supports the focus of a change initiative.

What is this phase?
This phase is typically the starting point when you and your change team have decided that you desire to make an improvement to an existing practice, infrastructure or intervention that you currently use or have in your work setting, such as a treatment program or an assessment (Kitson and Straus, 2013).
What if I already have identified the problem and know what I want to change in practice?
If you have already identified the evidence-informed practice or intervention that you want to integrate into your practice, this phase can help you review the practice gap in your setting to confirm that the knowledge you have chosen can fill this gap.
There are three components to this phase
- Identify the problem: Problems are identified differences between existing practices versus the desired practices in your setting.
- Determine the knowledge-to-practice gap: This “gap” refers to the difference between the knowledge of what the evidence shows will work and actual practice. Ideally, this type of knowledge should come from high-quality practice guidelines or knowledge syntheses such as systematic reviews. Once you define a knowledge-to-action gap, you can identify the practice change or intervention that can minimize the gap.
- Identify, review, select knowledge: “Knowledge” here refers to the best available evidence that you can use to apply to your problem and address the knowledge-to-practice gap that you and your team have identified. Evidence can be in the form of BPGs, knowledge syntheses, or policies.
SOURCES: Graham et al., 2006; RNAO 2012; Straus et al., 2009.
There are three components in this phase each of which are described below.
Identifying the problem or issue
How do you know you have a problem?
There are many ways to identify the problem. Look to information sources to help you identify the problem at multiple levels including:
- micro level (for example, health professionals)
- meso level (for example, a health-care organization)
- macro level (for example, the broader health system)

Micro level – the point of care
- Observation of staff
- Competency assessments (for example, knowledge questionnaires)
- Reflective practice
- Performance reviews
- Critical safety incidents
- Clinical audits
- Health outcomes

Meso level – the organization
- Needs assessments
- Accreditation results
- Electronic records
- Quality improvement indicators

Macro level – the health system
- Population data
- Epidemiological data
- National or regional databases
SOURCES: Kitson and Straus, 2013; RNAO, 2002; RNAO 2012.
Some problems are caused by multiple contributing factors at different levels. For example, medication errors can result from errors in the electronic health system, an oversight in the pharmaceutical department or a wrongly assigned prescription by a health professional.
Even if the error itself is simple, you may need to do more investigative work to find the root causes of the problem. You can use tools such as the “Five whys” approach or the cause-and-effect diagram in the “Additional resources” table at the end of this section).
Remember: Be sure you and your team clearly understand the problem or issue that needs to be addressed.
Here are some questions to help you identify and understand the problem area or issue:
- Is the problem a priority for the specific population affected?
- Who may gain or who may lose if this problem is addressed?
- What are the existing practices you would like to improve?
- How will addressing this problem improve existing practice?
- If there is more than one problem identified, which is the priority?
SOURCES: Knowledge Translation Canada, 2020; Mental Health Commission of Canada, 2014.
Determining the knowledge-to-practice gap (know-do gap) using best practice
Model your practices based on evidence such as BPGs, quality indicators, decision-making algorithms or systematic reviews.
Review the practices, policies, health outcomes, attitudes, knowledge and skills currently existing within your setting
Once you and your team have identified a problem or issue, you can determine the knowledge-to-practice gap. Here are some questions to help you identify this gap:
- What are the gaps between the best practice and current practice for the identified problem?
- In which contexts and to what extent do these gaps exist?
- Consider again, who may gain and who may lose if a particular gap is prioritized?
- Is there potential for bias depending on who is defining the problem? (For example, a hospital CEO and a nurse at the hospital may identify different problems to prioritize.)
SOURCE: Knowledge Translation Canada, 2020.
How do you assess the knowledge-to-practice gap and understand the size and nature of the gap?
- Use a systematic process for determining the size and nature of the gap. A gap (or opportunity) analysis allows for a detailed approach that uncovers multiple aspects of health-care delivery that may need to change, and creates an opportunity to change practice through the implementation of evidence.
- Use data, like survey results, informant interviews, chart audits or evaluation results, to help determine the size and nature of the gap. Results from your gap analysis can also help you identify resource needs and pinpoint interventions (Golden et al., 2017).
- A gap analysis may also help determine strengths, areas where best practices have been implemented in part – which would be good places to start – and facilitators and barriers to implementation.
- When determining the knowledge-to-practice gap, engage multiple persons involved in the change and encourage “dynamic dialogue” and candid discussions. This improves engagement, supports creative solutions and helps unite a team in improving care.
SOURCES: Golden et al., 2017; Holmes et al., 2018; Kitson and Straus, 2013; RNAO, 2012.
Remember: Persons and groups involved in the change may offer different knowledge sources and bring unique perspectives. Consider all aspects – and strive to reach a consensus before proceeding!
Prioritizing which knowledge-to-practice gap to address
If you and your change team identify multiple gaps, it can be helpful to determine prioritized areas of focus with input and feedback from others such as staff. To support decision-making regarding priority areas, the following questions can be helpful to discuss as a team.
- Is this gap an area of clinical concern?
- Does evidence exist to address this gap?
- Are baseline data available to indicate current outcomes?
- Is there enough interest from key personnel to support work on filling this gap?
- Does addressing this gap have the support of your senior leadership team?
- Does addressing this gap align with other local, regional or national activities?
- Would doing something be feasible, practical and desirable?
SOURCE: Adapted from Kitson and Straus, 2013.
Identify, review, and select the knowledge tool
For this section, you and your change team will identify, review and select knowledge tool(s) to help you address the knowledge-to-practice gap.
Knowledge tools such as BPGs are intended to support the effective implementation of your knowledge-to-practice gap. But not all knowledge tools are equally effective.
Ideal tool characteristics include an explicit statement of objectives, a description of who would use the tool, and instructions on how to use it, among other desirable features.
These are examples of knowledge tools:
- RNAO’s BPGs or other clinical practice guidelines
- Quality indicators
- Decision-making algorithms
- Systematic reviews
Some desirable features of a knowledge tool (Gagliardi et al., 2014):
- Tool objectives are stated.
- Target users are named.
- Instructions on tool use are provided.
- Methods used to develop the tool are described.
- The tool is based on a comprehensive search for content.
- The evidence upon which tool content is based is described.
- Sources of evidence are cited.
- The setting in which the tool was developed and in which the tool will be used is described.
- Those who intended to use the tool were involved in tool development.
- Methods used to evaluate the tool are described.
- The tool was pilot-tested with users.
- There are prospective plans to collect user feedback about the tool’s use and effects.
There are many clinical BPGs available online – but it’s important to note that not all knowledge tools reflect best practices. If creation of the tools did not require a rigorous approach to selecting and assessing the available evidence, the tools could be biased or unclear.
Examples of organizations that use rigorous methods to develop guidelines include AGREE Enterprise, Guidelines International Network, National Institute for Health and Care Excellence, Registered Nurses’ Association of Ontario and Scottish Intercollegiate Guidelines Network.
RNAO’s guidelines are created using the highest international standards for guideline development. Learn more about the guideline development methodology
Trustworthy knowledge tools should include references for the evidence presented and disclose any conflicts of interest. Financial, intellectual and other interests might lead knowledge tool developers to omit or downplay a health risk, overstate outcome effectiveness or provide misleading statistics. (Moore et al., 2017).
Remember: You and your colleagues must be able to trust the knowledge tool, believe that it adequately addresses the problem or gap and is suitable for your setting.
How do you and your change team select the right knowledge tool to address a problem/issue?
- Use a systematic process.
- Use a process for selecting the knowledge tool that helps you determine the quality and fit for your setting.
- In cases where there is more than one knowledge tool to be selected, be aware that some team members may have preferences based on past experiences. Beyond the criteria of quality and contextual fit, the group should reach a consensus regarding the final selection of the knowledge tool.
- Work as a team.
- Gather your team. Identify individuals who can help select the knowledge tool. This should include people who will be using the tool directly and may include people who understand research methods.
- Engage leaders. Engage formal and informal leaders, such as representatives from senior management teams, unit managers, local opinion leaders, quality/risk management and frontline staff.
- Listen to everyone’s concerns. Actively seek individuals who have initial doubts or concerns about the problem you want to address in your setting. Listen attentively, and (if possible) offer solutions that address their questions and doubts. Value their input and invite them to be part of this team.
- Ensure that everyone has a voice. Encourage members of the team to voice their perspectives regarding identifying the problem and selecting knowledge. To work cohesively, make sure you allocate enough time to discuss all concerns and claims regarding the proposed change.
Remember: It is important that everyone agree and can defend the choice of knowledge tool. (Bajnok et al., 2018b).
Why is this phase important?
This phase is important because it will help you and your change team to:
- understand the extent of the problem
- articulate the gap or need
- outline what needs to change in order to fill the gap or address the problem
- provide a clear rationale for addressing the problem that can be communicated to others
- select suitable knowledge tools or products to address the need.
- prioritize the most important problems or gaps to address
Case studies

Identificar el problema en la Fundación Cardioinfantil del Instituto de Cardiología (FCI-IC) para lograr la excelencia en la atención
La Fundación Cardioinfantil del Instituto de Cardiología (FCI-IC) es un hospital de 340 camas en Bogotá, Colombia. En Colombia, no era habitual que se usasen guías de buenas prácticas (GBP) en la asistencia enfermera; se unieron al programa de Centros Comprometidos con la Excelencia en Cuidados de RNAO (Best Practice Spotlight Organization® - BPSO®) con el objetivo de lograr la excelencia en los cuidados.
La FCI-IC disponía de datos de evaluación a lo largo de 10 años que revelaron problemas en ciertas áreas clínicas como la prevención de caídas y el cuidado de heridas. Realizaron una evaluación diagnóstica de referencia (basal) para determinar los problemas prioritarios que debían abordarse y seleccionar las guías y recomendaciones de buenas prácticas más adecuadas. Para ello, encuestaron a las partes interesadas para conocer mejor el uso que hacen de las herramientas de evaluación, la situación de las historias clínicas electrónicas, las prácticas clínicas habituales, como el uso de barandillas en la cama, y los datos de prevalencia.
Este proceso de valoración les llevó a seleccionar tres GBP de RNAO como herramientas de conocimiento: Prevención de caídas y lesiones derivadas de las caídas en las personas mayores, Valoración del riesgo y prevención de las úlceras por presión, y Valoración y manejo de úlceras del pie diabético.
Conducting gap analyses to successfully implement new clinical practices at Tilbury Manor
Tilbury Manor, a 75-resident long-term care home in Tilbury chose to focus on provincially-mandated “required programs” (fall prevention, skin and wound care, continence care, bowel management and pain management) when seeking to improve resident care.
They conducted a gap analysis to compare their current practices with the best practices outlined in related RNAO best practice guidelines. Their analysis included an assessment of clinical practices, policies and documentation systems. The results of the gap analysis helped them create specific action plans.
Tilbury Manor then formed project teams led by nurses and supported by a team of champions. These teams proceeded to educate staff, implement new clinical practices, conduct care reviews and conduct audits.
Multiple positive outcomes were reported as a result of implementing these best practices including reductions in reports of pain, less use of restraints, and less falls, pressure ulcers and urinary tract infections.
Practice tips
- Enlist the support of formal leaders such as managers, supervisors and chief nursing officers. Make sure they are involved or kept well-informed in all processes related to this phase.
- Work with your team to clearly articulate the problem.
- Think about which attitudes, knowledge, skills, behaviours, policies, outcomes are desired or needed to meet best practices.
- Select a knowledge tool through a systematic and participatory practice.
- Clarify the following:
- What is the knowledge-to-practice gap?
- Who needs to be involved to address this knowledge gap?
- What specific behaviours do those individuals or groups need to change to reduce the gap?
- How does this differ from what those individuals or groups are currently doing?
- When and where do these behaviours need to be performed?
- Engage champions and recruit staff members who express a need for change. Work as a team and split up the work so that small groups look at different issues such as documentation, education and communication.
- Choose someone who has good facilitation skills to help your group identify gaps in practice and processes.
SOURCES: Bajnok et al., 2018b; Grimshaw and Presseau, 2018; Kitson and Straus, 2013.
Download the worksheet "Identifying the problem area of issue".
KTA tools

Applying pragmatic and valid tools can support change teams to accurately measure the identified problem or determine the know-do gap and strengthen their understanding of these components. Using these tools can also help change teams prepare for the next action cycle phase, “Adapt knowledge to the local context”.
For each tool, we provide two documents:
- a summary page that includes the tool’s purpose, description and applicable action cycle phases
- a companion document that details the tools’ pragmatic and psychometric properties
Additional resources to support the use of KTA tools:
Click here to view two summary tables that describe all of the tools included in the Leading Change Toolkit, detail what they measure and identify in which of the KTA action cycle phase or phases they can be applied.
Click here to read more about considerations for using KTA tools by change teams including the how-to's of selecting a tool, implementing it, and determining the next steps for follow-up.
Valid KTA tools
Check your progress
- You have engaged a group of individuals, including people with direct experience and knowledge about the problem/gap to work through this step.
- You have taken into account the concerns, doubts and questions raised by individuals, and have respectfully addressed their concerns.
- You have involved formal leaders or kept them well-informed.
- You have used stated the problems and gaps, and used data to support your findings.
- You have used a systematic approach and have a clear rationale to support the choice of the knowledge tool.
- You could confidently defend your choice of the knowledge tool as high-quality and suitable for the needs of staff and other stakeholders.
- You have identified priorities to address.
Linking this phase to other framework components
Linking this phase to the elements of the Social Movement Action Framework
You and your change team’s capacity in the “Identifying the problem” phase may be enhanced or accelerated by adding in some of the elements of the Social Movement Action (SMA) Framework, as the two frameworks are complementary. In addition to the linking example described earlier in this section, there can be many other points of connection between the two frameworks. Below are three examples for you to consider:
- Urgent need to take action: To identify priority areas for change, change teams can also consider areas of shared concern or strongly desired change. The shared concern or strongly desired change should be seen as credible, valued and in need of urgent action to address. This urgency creates a mounting pressure and support for change that can act as a strong foundation or starting point towards action.
- Change is valued and necessary: When a change team identifies a problem or shared concern that is valued and recognized as positively impacting outcomes at the micro, meso, and/or macro levels, it can leverage people to start supporting the cause and becoming engaged in the change.
- Framing: Framing or positioning the identified problem in ways that emphasize it as a credible change that matters to people and can positively impact outcomes can be a value-add in this planning phase of change.
For more discussion about the dynamic links between the elements of the SMA Framework to the KTA Framework, see the section "Two complementary frameworks".
Getting ready for the next phase: Once you have identified your problem and selected the practice you want to change or implement, you are now ready to assess the local context. This upcoming phase can help you and your change team think about how your practice change can be effectively used in your setting, and to assess whether your setting is ready for this practice change.
More resources
Want to learn more about using the strategies of the SMA and KTA frameworks to support your change? Sign up for the RNAO Best Practice Champions training course.