Case studies
Social Movement Action Framework
Building a global collective identity to advance knowledge uptake and sustainability - the RNAO Best Practice Spotlight Organization (BPSO) Program
RNAO's Best Practice Spotlight Organization (BPSO) program has integrated a collective identity of knowledge champions to advance evidence uptake and sustainability.
|
The Best Practice Spotlight Organization® (BPSO®) Program (https://rnao.ca/bpg/bpso) has global reach and impact that is sustained by many factors, including the development of collective identity that promotes an evidence-based culture. The BPSO logo, as a tangible representation of a collective identity, is displayed in individual sites to indicate they are BPSO units. This visibility motivates and inspires nurses and other staff to use best practice guidelines (BPG) to support the health and well-being of staff, patients/persons and their families. Participation and membership in the international BPSO network further the ties and pride of BPSO and builds the collective identity (Grinspun & Bajnok, 2018).
Within organizations, individual BPSOs nurture Best Practice (BP) Champions (https://rnao.ca/bpg/get-involved/champions) who take on leadership roles to support the planning, implementation, evaluation and sustainability of BPGs. Nurses and other staff members develop a collective identity based on a culture of integrating evidence-based practice to achieve excellence in care. The visibility of BP Champions is seen when staff where BPSO-branded clothing items, and pins that are awarded at the completion of the Best Practice Champions’ training workshop (see the examples below of social media posts of BPSO-branded t-shirts and a pinning ceremony of new champions by RNAO CEO, Dr. Doris Grinspun) (Grinspun & Bajnok, 2018). |

Building a collective identity to foster an anti-bullying culture
As part of a school anti-bullying campaign for children of military families in the United States, social movement participants used collective identity to promote anti-bullying messages. Read more in this case study.
As part of a grassroots anti-bullying campaign for children of military families in schools in the United States, social movement participants used collective identity to promote anti-bullying messages. Collective identity activities taken by school staff, parents and community members to promote the message "Because Nice Matters" included:
- designing and using posters, artwork and t-shirts to publicize their communication messages
- selecting and using the colours black and purple to unify their campaign
- engaging staff and students in the initiative
- having local businesses wear t-shirts with anti-bullying messaging as a sign of community support (de Pedro et al., 2017).

Guiding best practice guidelines (BPG) implementation with BPSO implementation teams
To support the effective implementation of BPGs, Best Practice Spotlight Organizations® (BPSOs®) create change teams that operate as core leadership structures to support evidence uptake and sustainability. Learn more in this case study.
To support the effective implementation of BPGs, Best Practice Spotlight Organizations® (BPSOs®) create change teams that operate as core leadership structures to support evidence uptake and sustainability. Their roles in the core leadership structure can include:
- selecting recommendations
- developing an action plan
- mobilizing implementation strategies
- supporting adherence to a practice change
- engaging in monitoring and evaluation activities
- taking active steps to support sustainability
As champions, one role of BPSOs is to compare their current practice to the guideline recommendations to see how the current practice can be maintained, strengthened or changed. Taking a “can do” attitude, they actively collaborate with their peers throughout the change process, and value and welcome their input and ideas. They take on leadership roles to support evidence-based practice change in collaboration with nurses, other staff and others (Bajnok et al., 2018a).

Knowledge-to-Action Framework
Applying the Knowledge-to-Action Framework to reduce wound infections at Perley Health
A case study on reducing wound infections at Perley Health in Ottawa, Ontario to advance best practices using the Knowledge-to-Action framework.
Perley Health is a designate Long-Term Care Best Practice Spotlight Organization® (BPSO®) which demonstrates a strong commitment to providing evidence-based care. During the pandemic, the team identified skin and wound infection as a clinical concern among their residents. Consistent with the literature, residents at Perley Health experiencing comorbid medical conditions such as frailty, diabetes, and arterial and venous insufficiency were at increased risk for chronic wound infections [1]. Chronic wounds are a prime environment for bacteria, including biofilm, making wound infection a common problem [2] [3]. Managing biofilm, which can affect wound healing by creating chronic inflammation or infection [3], becomes crucial as up to 80 per cent of infections are caused by this type of bacteria [4] [5].
To adopt and integrate best practices, the team at Perley Health decided to implement the Assessment and Management of Pressure Injuries for the Interprofessional Team best practice guideline (BPG). To support a systematic approach to change, four of the action cycle phases of the Knowledge-to-Action Framework, from the Leading Change Toolkit [6] are highlighted below.
Identify the problem
Perley Health’s wound care protocol was audited and the following gaps were identified based on current evidence:
- Aseptic wound cleansing technic could be improved, as nonsterile gauze was used for wound cleansing.
- Wound cleaning solution was not effective to manage microbial load in chronic wounds
- Baseline wound infection data were collected on the number of infected wounds within the organization each month over three years and is ongoing
Adapt to local context
The project was supported by key formal and informal leaders within the organization including the Nurse Specialized in Wounds, Ostomy and continence (NSWOC), the Director of Clinical Practice, a team of wound care champions, the IPAC team and material management. Staff was motivated to improve resident outcomes by lowering infection rates which facilitated the project but many continued to use old supplies so as to not waste material. Providing the rationale for the change and associated best practices improved knowledge uptake, as did removing old supplies to cut down on confusion. Barriers the team encountered included staff turnover and educating new team members.
Select, tailor, implement interventions
The interventions listed below were selected, tailored and implemented based on the evidence that was adapted to the local context. They were purposely chosen to support the clinical teams’ needs on busy units and to creatively overcome staffing challenges. Interventions included:
- use of a wound cleanser containing an antimicrobial
- use of sterile equipment for wound care, including sterile gauze
- creation of a wound-cleansing protocol was created to reflect best practice
- updating and approval of a policy by the Risk Assessment and Prevention of Pressure Ulcers team in collaboration with the director of clinical practice
Perley Health also created and delivered education in two formats designed to be accessible to front-line staff:
- Just-in-Time education was provided on every unit, on every shift, to registered staff by the NSWOC on all shift sets, over a one-month period. Wound care champions were available on each shift to aid in learning and answer additional questions to support the team’s needs.
- A continuing education online learning module was created and uploaded onto Perley Health’s Surge learning platform. Training is included in new hire onboarding and mandatory for yearly education.
Image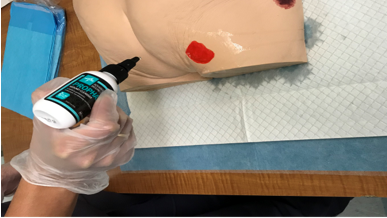
An RPN demonstrating how to cleanse a wound using wound cleanser at Perley Health
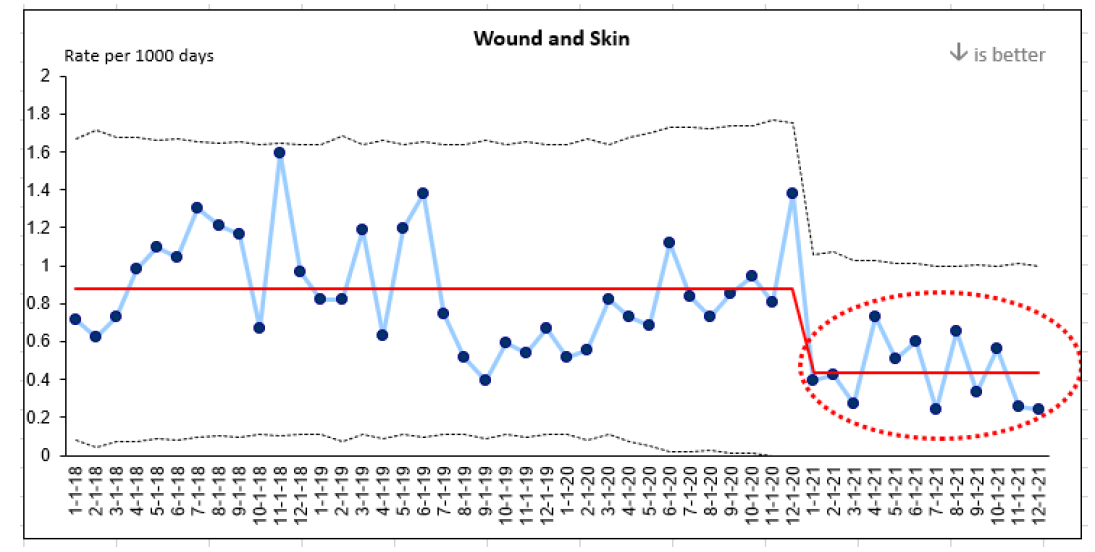
Evaluate outcomes
Evaluation indicators were selected to determine the impact of the implementation interventions when compared to baseline data, including the rate of wound and skin infections per 1,000 days. A 50 per cent reduction in wound infections was identified following the implementation of the identified change strategies and education above.
This graph represents four years of data collection on wound infections at Perley Health. Three years of baseline data and one year of post-implementation data are highlighted in red.
References
- Azevedo, M., Lisboa, C., & Rodrigues, A. (2020). Chronic wounds and novel therapeutic approaches. British Journal of Community Nursing, 25 (12), S26-s32.
- Landis, S.J. (2008). Chronic Wound Infection and Antimicrobial Use. Advances in Skin & Wound Care, 21 (11), p 531-540.
- Registered Nurses’ Association of Ontario (2016). Clinical best practice guidelines: Assessment and management of pressure injuries for the interprofessional team (3rd ed.). Registered Nurses’ Association of Ontario: Toronto, ON.
- Jamal, M., Ahmad, W., Andleeb, S., Jalil, F., Imran, M., Nawaz. M., Hussain, T., Ali, M., Rafiq, M., & Kamil, M.A. (2018). Bacterial biofilm and associated infections. J Chin Med Assoc. 81(1): 7-11.
- Murphy, C., Atkin, L., Swanson, T., Tachi, M., Tan, Y.K., De Ceniga, M.V., Weir, D., Wolcott, R., Ĉernohorská, J., Ciprandi, G., Dissemond, J., James, G.A., Hurlow, J., Lázaro MartÍnez, J.L., Mrozikiewicz-Rakowska, B., & Wilson, P. (2020). Defying hard-to-heal wounds with an early antibiofilm intervention strategy: wound hygiene. J Wound Care, (Sup3b):S1-S26.
- Registered Nurses’ Association of Ontario (2022). Leading change toolkit: Knowledge-to-action framework. https://rnao.ca/leading-change-toolkit Registered Nurses’ Association of Ontario: Toronto, ON.

Overcoming barriers to evidence-based practice – Lessons learned from DongZhiMen Hospital and Beijing University of Chinese Medicine (BUCM) School of Nursing
DongZhiMen Hospital and Beijing University of Chinese Medicine (BUCM) School of Nursing are international BPSOs in Beijing, China. Staff at the sites identified barriers to the use of evidence in practice including heavy workloads, cultural differences and reluctant attitudes about using evidence to inform practice.
DongZhiMen Hospital and Beijing University of Chinese Medicine (BUCM) School of Nursing are international BPSOs in Beijing, China. They identified barriers to the use of evidence in practice including heavy workloads, cultural differences and reluctant attitudes about using evidence to inform practice. The assessment and identification of barriers allowed change teams to develop effective strategies for implementation with the input of stakeholders.
For example, for the implementation of the RNAO best practice guideline Assessment and management of foot ulcers for people with diabetes, barriers included
- nursing shortages across China,
- a lack of training to support the development of knowledge and skills in evidence-based nursing practice,
- the costs of guideline implementation. and
- practice recommendations that exceeded local nursing scope.
SOURCE: Transforming Nursing Through Knowledge, 2018.

Facilitating an evidence-based culture at Unity Health Toronto - St. Michael’s Hospital
Unity Health Toronto - St. Michael’s Hospital, a Best Practice Spotlight Organization® (BPSO®) has embedded evidence-based practices into its culture and daily work processes as part of its corporate strategy.
Unity Health Toronto - St. Michael’s Hospital, a Best Practice Spotlight Organization® (BPSO®) in Toronto, Canada, has embedded evidence-based practices into its culture and daily work processes. Evidence-based practice is part of the hospital’s corporate strategy. It has invested resources to build a critical mass (over 30 per cent) of staff members who are best practice champions.
The hospital also provides multiple capacity-building opportunities, including a community of practice, boot camps, booster sessions and mentorship. The annual Nursing Week Gallery Walk, depicted in the image above, is just one way that St. Michael’s Hospital profiles the work of champions and others dedicated to using evidence to inform change initiatives.
SOURCE: Transforming Nursing Through Knowledge, 2018.

Engaging Persons with Lived Experiences
Engaging Patient Family Advisors to advance guideline implementation at Scarborough Health Network
A case study about the integration of patient family advisors at Scarborough Health Network to enhance community engagement and health equity.
Scarborough Health Network (SHN) (Home - Scarborough Health Network (shn.ca) is an organization pursuing Best Practice Spotlight Organization® (BPSO®) designation in Scarborough, Ontario, Canada. Patient Family Advisors (PFAs) are a vital part of SHN’s philosophy of care, representing the diverse community SHN serves. A key element of the PFA role is sharing lived experiences with SHN staff and the Scarborough community.
SHN has demonstrated commitment to the role of PFAs within their organization by creating a new department for health equity, patient and community engagement (HEPCE). This department focuses on:
- recruiting, onboarding, managing, recognizing and retaining PFAs
- educating staff on best practices related to engaging with PFAs
During recruitment and onboarding, the HEPCE and current PFAs educate potential PFAs about the role’s scope and expectations. All PFAs are also provided with information on how to share their patient or caregiver story with their audience.
PFAs have played an important role in SHN’s BPSO committee. Indeed, one PFA has been integral to the process of recruiting and engaging champions at SHN throughout the COVID-19 pandemic’s health human resources (HHR) crisis. Their role has included participating in champions’ virtual drop-in sessions (2020-2021) and in-person roadshows (2022).
Champion roadshows are events during, which SHN practice leaders and PFAs promote the BPSO program, share best practice guidelines and recruit champions around the organization, without asking busy staff members to leave their units.
The PFA also supported the recruitment and engagement of champions by:
- collaborating with other champions and working group members to plan champions’ drop-in sessions and roadshows
- working alongside the team to plan safe spaces for staff and PFAs to share their stories
- sharing stories of positive experiences with staff members in relation to the impact of best practices (for example, RNAO’s Person and Family Centred-Care best practice guideline) on their experience
Staff members have reported being motivated to become best practice champions after attending a champion’s roadshow. SHN has also consistently gained champions during the HHR crisis and maintains at least 15 per cent of nursing staff as best practice champions.
The PFA’s role was vital to demonstrating the lasting impact of best practices. They have expressed feeling empowered by their role in BPSO work, expressing that the work helped them find their voice and become part of the movement to promote and implement best practices.
Overall, PFAs play an essential – and dual – role in supporting the implementation of best practices at SHN. In line with person- and family-centred care, PFAs assume an outward-facing role in shaping the implementation of best practices and SHN’s values. In addition, they also act in an inward-facing role to support the bolstering of champions.
To learn more about the PFA role at SHN, please visit the following link: Patient Family Advisors.
Shared with permission by Scarborough Health Network

Co-designing change through the active engagement of persons with lived experience - Holland Bloorview Kids Rehabilitation Hospital
Case study - Holland Bloorview
Holland Bloorview Kids Rehabilitation Hospital (Holland Bloorview) is a designated Best Practice Spotlight Organization® (BPSO®) in Toronto, Canada. Holland Bloorview has an award-winning Family Leadership Program (FLP), through which family leaders partner with the organization and the Bloorview Research Institute to co-design, shape and improve services, programs and policies.
These family leaders are families and caregivers who have received services at Holland Bloorview and have lived experiences of paediatric disability. Their roles include mentoring other families, acting as advisors to committees and working groups, and co-teaching workshops to students and other families.
One example of a successful implementation co-design within Holland Broadview is the ENFit™ Working Group. This interprofessional team works on the adoption of a new type of connection on products used for enteral feeding – or feeding directly through the stomach or intestine via a tube. By introducing the ENFit™ system, a best practice safety standard, the working group plans to reduce the risk of disconnecting the feeding tube from other medical tubes. This in turn decreases harm to children and youth who require enteral feeding.
The working group invited a family member and leader whose son had received services at Holland Bloorview. This family member had significant lived experience with enteral feeding management, enteral medication administration, and other complexities associated with enteral products. During the meetings, the potential impacts on persons and families were emphasized. The working group engaged the family member by:
- co-creating the implementation plan
- involving them in a failure mode and effects analysis highlighting the impact of the feeding tube supplies on transitions to home, school and other care settings
- working with the family member to advocate for safe transitions within the provincial pediatric system, which led to the development of the Ontario Pediatric ENFit™ Group
To learn more about Holland Bloorview’s experience in partnering with families in a co-design process, watch their 38-minute webinar: The Power of Family Partnerships
Shared with permission from Holland Bloorview

Integrating patient partners in change – Lessons learned from Kidney Health Australia
Kidnney Health Australia case study
In early 2018, Kidney Health Australia (KHA) developed a guideline for managing percutaneous renal biopsies for individuals with chronic kidney disease (Scholes-Robertson et al., 2019). KHA included 40 persons from across Australia with lived experience of chronic kidney disease and their caregivers – “patient partners”. KHA asked patient partners to prioritize which topics were most important to them during a percutaneous renal biopsy.
Patient partners valued: minimizing discomfort and disruption, protecting their kidneys, enabling self-management, and making sure that support for families and caregivers would be available. They indicated that all of this would help alleviate anxiety and avoid undue stress. Their voices were heard, and KHA effectively incorporated these suggestions in guideline development.
Notably, there were marked differences between the priorities identified by the content experts on the guideline development working group, versus what the patient partners perceived to be important to their health and wellbeing, as shown in the table below.
|
Topics prioritized by content experts |
Topics prioritized by patient partners |
|
|

