Case studies
Social Movement Action Framework
Advancing knowledge uptake and sustainability through RNAO's Best Practice Champions Network®
The Best Practice Champions Network® has been engaging change agents for over two decades to facilitate connection, a sense of belonging and a place to continue the implementation of best practice guidelines.
Launched in 2002, the RNAO Best Practice Champions Network® supports the active engagement of volunteer peer Best Practice Champions in knowledge exchange amongst one another, and between them and RNAO. Through this international network, more than 100,000 champions access tools and strategies such as workshops, webinars and online modules (Grinspun, 2018).

Maintaining momentum to achieve excellence - Unity Health Toronto: St. Michael's Hospital
To keep the momentum as a Best Practice Spotlight Organization® (BPSO®), Unity Health Toronto: St. Michael’s Hospital engaged their Professional Practice team as change leaders. Read more in this case study.
To keep the momentum as a Best Practice Spotlight Organization® (BPSO®) implementing, evaluating and sustaining RNAO best practice guidelines (BPGs), Unity Health Toronto: St. Michael’s Hospital, https://rnao.ca/bpg/bpso/st-michaels-hospital, an acute care facility in Toronto, Ontario, Canada engaged their Professional Practice team as change leaders. Strategies the Professional Practice team have used to maintain momentum include:
- profiling the activities, leadership and achievements of their champions and other change agents
- using newsletters, posters and pins to promote BPSO and increase its visibility
- participating in poster galleries and nursing rounds
- publishing multiple articles in scholarly and professional journals to highlight key accomplishments and deliverables
- creating and using an intranet site to update staff on BPSO activities (Ferris, Jeffs, Krock, & Skiffington, 2018).

Sustaining a health system change with momentum
To create system level changes in health-care in the United Kingdom, momentum was fostered to achieve goals. Read more in this case study.
The Health as a Social Movement project for the National Health Services (NHS) developed the Programme Theory of Change to create system-level changes in health care in the United Kingdom.
The project used this theoretical model to provide impetus for change by defining goals for the change. These goals included connecting individuals, groups and organizations acting as change agents with the health system to mobilize local action for health.
Momentum played a pivotal role in achieving system change and transformation. Indicators of momentum included:
- an increase in social connectedness of individuals, groups and/or organizations
- higher levels of control, resourcefulness and resilience in the community
- an increase in change agents’ confidence and influence over the health system
The sustained momentum arising from the individual and collective action aimed to support a preventable and sustainable health system, characterized as having:
- improvements in local services
- an integration of determinants of health into service provision
- higher levels of health and well-being (Arnold et al., 2018).

Knowledge-to-Action Framework
Implementing effective interventions for drug and alcohol use using Screening, Brief Intervention and Referral to Treatment (SBIRT)
Evidence-based interventions to support the development of a screening, brief intervention and referral to treatment (SBIRT) for persons who use drugs and alcohol.
Screening, Brief Intervention, and Referral to Treatment (SBIRT) is endorsed by the Substance Abuse and Mental Health Services Administration as an effective intervention for drug and alcohol use. SBIRT has been implemented in multiple health-care settings including acute care.
Implementation leaders were asked to identify barriers, facilitators, as well as implementation strategies that would be most helpful. From this review, implementation leaders perceived that providing ongoing consultation to clinicians for using SBIRT, distributing educational materials to clinicians, and conducting audits and providing feedback were the most helpful.
All implementation leaders voiced the value of available training resources, and peer support as they moved through the implementation process.
Implementation leaders felt more confident leading change in the future due to the knowledge and skills they developed during SBIRT implementation. They also learned the importance of leveraging support from other interprofessional team members, such as social workers and clinical educators.
Read more about it here. Learn more about SBIRT here. Or, review our best practice guideline, Engaging Clients Who Use Substances.

Adapting BPG recommendations to a public health context – Insights from Toronto Public Health
Toronto Public Health – a Best Practice Spotlight Organization® (BPSO®) - has adapted several RNAO best practice guidelines (BPGs) to align with a population health approach.
Toronto Public Health – a Best Practice Spotlight Organization® (BPSO®) in Toronto, Canada – has implemented several RNAO best practice guidelines (BPGs), including Woman Abuse: Screening, Identification and Initial Response (2005) and Preventing and Addressing Abuse and Neglect of Older Adults (2014). Because some practice recommendations in these guidelines focus on the individual person or patient level, they didn’t always align with Toronto Public Health’s population health approach.
To adapt recommendations to the public health context, the change team completed a literature review to explore definitions and adapt strategies to align with the model of care delivery and health promotion philosophy.
Another approach that was taken by Toronto Public Health: piloting BPG recommendations within one small program team. The team would then evaluate the implementation until successful, consistent with the Plan-Do-Study-Act approach). Once successful, the intervention was scaled up within the organization to other programs and teams (Timmings et al., 2018).

Adapting BPG recommendations to a Chinese acute care context to reform care delivery– lessons learned from DongZhiMen Hospital
Care practices were revised using adapted evidence-based best practice guidelines in an acute care facility in Beijing, China.
DongZhiMen Hospital – a BPSO in Beijing China – was motivated to reform care delivery through the use of RNAO BPGs. While best practice recommendations provided general guidance, DongZhimen Hospital identified the need to translate these statements into detailed instructions and parameters tailored to their specific hospital context.
To adapt statements to their context, they translated the guideline into Chinese. A multidisciplinary team then worked through the initial steps of the Knowledge-to-Action Framework. This involved:
- reviewing carefully the evidence to thoroughly understand the intent of the recommendations
- conducting a comprehensive gap analysis
- interviewing staff members and others to identify facilitators and barriers to the use of the BPG.
Using this information, the team was able to create specific, clinical nursing practice standards derived from the recommendations and relevant to their context (Hailing and Runxi, 2018).

Engaging Persons with Lived Experiences
Holland Bloorview Kids Rehabilitation Hospital: Co-designing change through the active engagement of persons with lived experience
A case study from Holland Bloorview Kids Rehabilitation Hospital focused on engaging persons with lived experience in a change process.
Holland Bloorview Kids Rehabilitation Hospital (hereafter referred to as Holland Bloorview) is a designated Best Practice Spotlight Organization® (BPSO®) in Toronto, Ontario, Canada. Holland Bloorview has an award-winning Family Leadership Program (FLP), through which family leaders partner with the organization and the Bloorview Research Institute to co-design, shape, and improve services, programs, and policies. Family leaders are families and caregivers who have received services at Holland Bloorview, and have lived experiences of paediatric disability. Family leaders’ roles include being a mentor to other families, an advisor to committees and working groups, and faculty who co-teach workshops to students and other families.
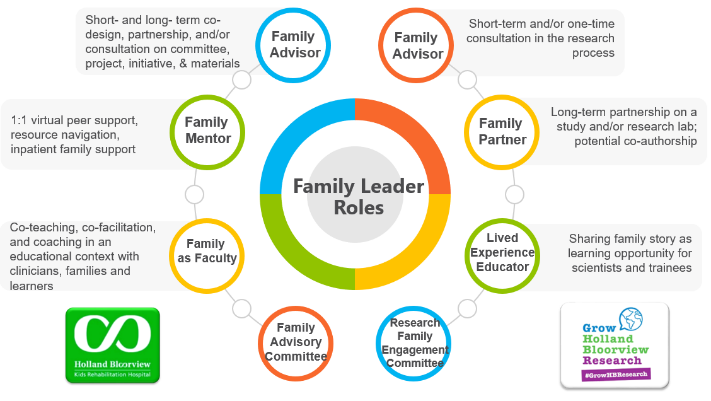
Family Leader Roles at Holland Bloorview. Photo provided with permission by Holland Bloorview Kids Rehabilitation Hospital.
The ENFit™ Working Group is an example of a successful implementation co-design process within Holland Bloorview. The ENFit™ Working Group is an interprofessional team working on the adoption of a new type of connection on products used for enteral feeding [feeding directly through the stomach or intestine via a tube]. By introducing the ENFit™ system, a best practice safety standard, the working group plans to reduce the risk of disconnecting the feeding tube from other medical tubes, and thus decrease harm to children and youth who require enteral feeding.
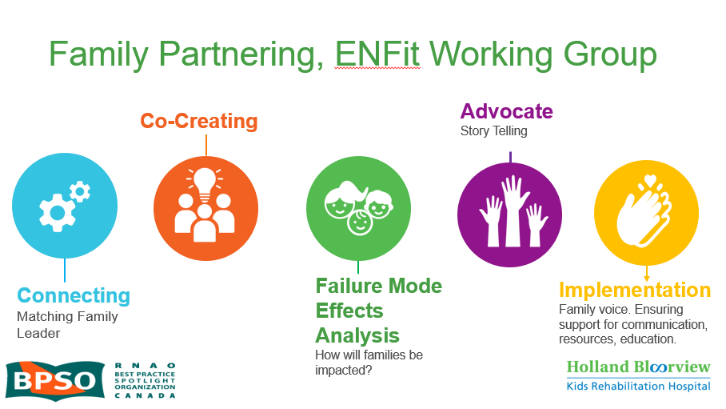
Family Partnering with the EnFit Working Group. Photo provided with permission by Holland Bloorview Kids Rehabilitation Hospital.
The working group invited a family member and leader whose son had received services at Holland Bloorview. This family member had significant lived experience with enteral feeding management, enteral medication administration, and other complexities associated with enteral products. During the meetings, great attention was given to the potential impacts on persons and families. The group engaged the family member by:
- co-creating the implementation plan
- involving them in a failure mode affects analysis, which highlighted the impact of the feeding tube supplies on transitions to home, school, and other care settings
- working with the family member to advocate for safe transitions within the provincial pediatric system, which led to the development of the Ontario Pediatric ENFit™ Group
To learn more about Holland Bloorview’s experience in partnering with families in a co-design process, watch their 38-minute webinar: The Power of Family Partnerships.

