Case studies
Social Movement Action Framework
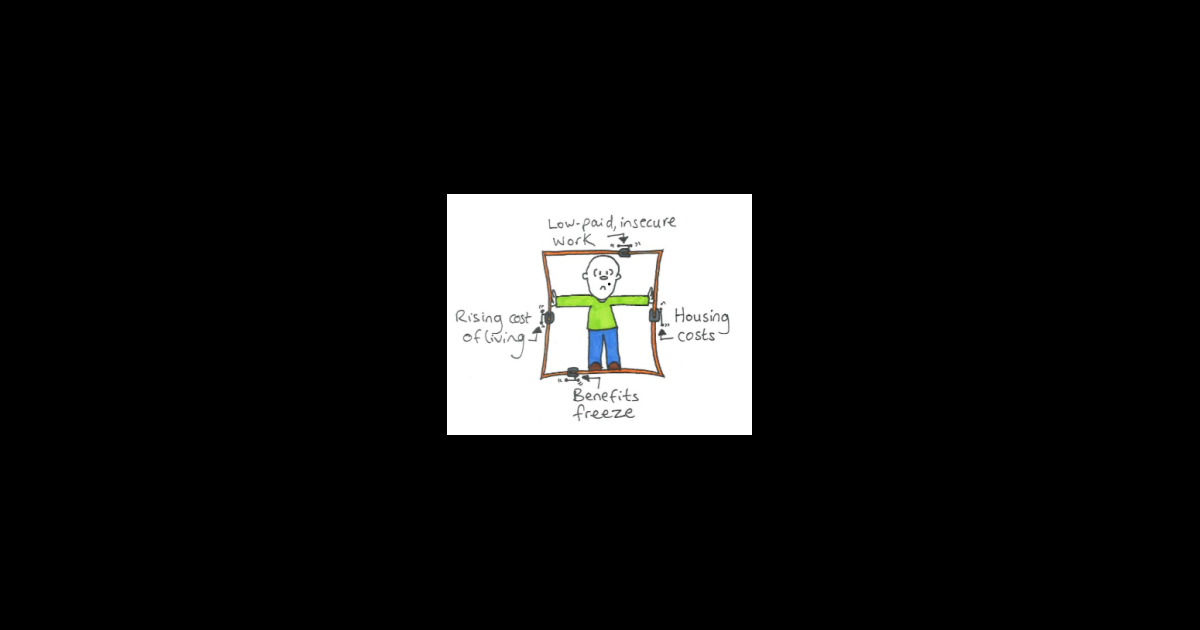
Doodling to frame the issue of poverty
Doodles are a creative expression of framing to position an issue and build meaning. Learn morew in this case study.
Here is an example of a doodle used to frame the issue of poverty. The notion of people being "locked in" by circumstances outside their control is a powerful metaphor. This doodle shows some of the main factors that combine to restrict and restrain people, locking them into poverty. (Joseph Roundtree Foundation)
Engaging champions' narratives
This RNAO champions training program used storytelling, metaphors, collective artwork and personal narratives to frame the importance of person-and family-centred care. Learn more
This RNAO champions training program used storytelling, metaphors, collective artwork and personal narratives to frame the importance of person-and family-centred care.
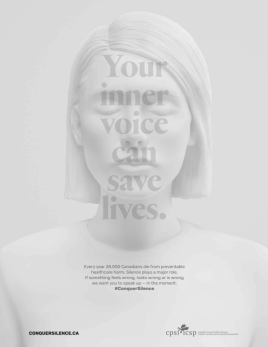
Using images and messages for a patient safety campaign
The Canadian Patient Safety Institute’s #ConquerSilence campaign uses images and powerful messaging to frame patient safety issues. Read more in this case study.
The Canadian Patient Safety Institute’s #ConquerSilence campaign uses images and powerful messaging to frame patient safety issues. The campaign includes webinars, podcasts, social media content and a communications toolkit.
Knowledge-to-Action Framework
Sustaining the Assessment and Management of Pain Best Practice Guideline across a multi-site long-term care home
The Region of Peel, a Best Practice Spotlight Organization® (BPSO®), has sustained the implementation of the Assessment and Management of Pain best practice guideline (BPG) for almost a decade.
The Region of Peel, an RNAO Best Practice Spotlight Organization® (BPSO®) started implementing the RNAO Assessment and Management of Pain best practice guideline (BPG) in 2014 and has sustained its use since then. For example, in their 2019 BPSO annual report, they cited a continuous downward trend in the number of clients who reported a worsening of their pain. Pain experienced by the residents was better controlled, and the staff was found to assess, identify, and manage pain better by using the BPG.
Their keys to success include:
- building on what works (for example, existing practices and policies)
- empowering champions and growing their champion network
- involving residents and families
- gaining support from leaders and partners including RNAO, Peel of Region Leadership, Health Quality Ontario).
- collaborating with an interdisciplinary team
- conducting a formal sustainability evaluation
To learn more about The Region of Peel’s journey in sustaining the use of the Assessing and Managing Pain BPG, along with other BPGs, check out this webinar.
Engaging Persons with Lived Experiences
Engaging Patient Family Advisors to advance guideline implementation at Scarborough Health Network
A case study about the integration of patient family advisors at Scarborough Health Network to enhance community engagement and health equity.
Scarborough Health Network (SHN) (Home - Scarborough Health Network (shn.ca) is an organization pursuing Best Practice Spotlight Organization® (BPSO®) designation in Scarborough, Ontario, Canada. Patient Family Advisors (PFAs) are a vital part of SHN’s philosophy of care, representing the diverse community SHN serves. A key element of the PFA role is sharing lived experiences with SHN staff and the Scarborough community.
SHN has demonstrated commitment to the role of PFAs within their organization by creating a new department for health equity, patient and community engagement (HEPCE). This department focuses on:
- recruiting, onboarding, managing, recognizing and retaining PFAs
- educating staff on best practices related to engaging with PFAs
During recruitment and onboarding, the HEPCE and current PFAs educate potential PFAs about the role’s scope and expectations. All PFAs are also provided with information on how to share their patient or caregiver story with their audience.
PFAs have played an important role in SHN’s BPSO committee. Indeed, one PFA has been integral to the process of recruiting and engaging champions at SHN throughout the COVID-19 pandemic’s health human resources (HHR) crisis. Their role has included participating in champions’ virtual drop-in sessions (2020-2021) and in-person roadshows (2022).
Champion roadshows are events during, which SHN practice leaders and PFAs promote the BPSO program, share best practice guidelines and recruit champions around the organization, without asking busy staff members to leave their units.
The PFA also supported the recruitment and engagement of champions by:
- collaborating with other champions and working group members to plan champions’ drop-in sessions and roadshows
- working alongside the team to plan safe spaces for staff and PFAs to share their stories
- sharing stories of positive experiences with staff members in relation to the impact of best practices (for example, RNAO’s Person and Family Centred-Care best practice guideline) on their experience
Staff members have reported being motivated to become best practice champions after attending a champion’s roadshow. SHN has also consistently gained champions during the HHR crisis and maintains at least 15 per cent of nursing staff as best practice champions.
The PFA’s role was vital to demonstrating the lasting impact of best practices. They have expressed feeling empowered by their role in BPSO work, expressing that the work helped them find their voice and become part of the movement to promote and implement best practices.
Overall, PFAs play an essential – and dual – role in supporting the implementation of best practices at SHN. In line with person- and family-centred care, PFAs assume an outward-facing role in shaping the implementation of best practices and SHN’s values. In addition, they also act in an inward-facing role to support the bolstering of champions.
To learn more about the PFA role at SHN, please visit the following link: Patient Family Advisors.
Shared with permission by Scarborough Health Network

Co-designing change through the active engagement of persons with lived experience - Holland Bloorview Kids Rehabilitation Hospital
Case study - Holland Bloorview
Holland Bloorview Kids Rehabilitation Hospital (Holland Bloorview) is a designated Best Practice Spotlight Organization® (BPSO®) in Toronto, Canada. Holland Bloorview has an award-winning Family Leadership Program (FLP), through which family leaders partner with the organization and the Bloorview Research Institute to co-design, shape and improve services, programs and policies.
These family leaders are families and caregivers who have received services at Holland Bloorview and have lived experiences of paediatric disability. Their roles include mentoring other families, acting as advisors to committees and working groups, and co-teaching workshops to students and other families.
One example of a successful implementation co-design within Holland Broadview is the ENFit™ Working Group. This interprofessional team works on the adoption of a new type of connection on products used for enteral feeding – or feeding directly through the stomach or intestine via a tube. By introducing the ENFit™ system, a best practice safety standard, the working group plans to reduce the risk of disconnecting the feeding tube from other medical tubes. This in turn decreases harm to children and youth who require enteral feeding.
The working group invited a family member and leader whose son had received services at Holland Bloorview. This family member had significant lived experience with enteral feeding management, enteral medication administration, and other complexities associated with enteral products. During the meetings, the potential impacts on persons and families were emphasized. The working group engaged the family member by:
- co-creating the implementation plan
- involving them in a failure mode and effects analysis highlighting the impact of the feeding tube supplies on transitions to home, school and other care settings
- working with the family member to advocate for safe transitions within the provincial pediatric system, which led to the development of the Ontario Pediatric ENFit™ Group
To learn more about Holland Bloorview’s experience in partnering with families in a co-design process, watch their 38-minute webinar: The Power of Family Partnerships
Shared with permission from Holland Bloorview

Integrating patient partners in change – Lessons learned from Kidney Health Australia
Kidnney Health Australia case study
In early 2018, Kidney Health Australia (KHA) developed a guideline for managing percutaneous renal biopsies for individuals with chronic kidney disease (Scholes-Robertson et al., 2019). KHA included 40 persons from across Australia with lived experience of chronic kidney disease and their caregivers – “patient partners”. KHA asked patient partners to prioritize which topics were most important to them during a percutaneous renal biopsy.
Patient partners valued: minimizing discomfort and disruption, protecting their kidneys, enabling self-management, and making sure that support for families and caregivers would be available. They indicated that all of this would help alleviate anxiety and avoid undue stress. Their voices were heard, and KHA effectively incorporated these suggestions in guideline development.
Notably, there were marked differences between the priorities identified by the content experts on the guideline development working group, versus what the patient partners perceived to be important to their health and wellbeing, as shown in the table below.
|
Topics prioritized by content experts |
Topics prioritized by patient partners |
|
|

