Case studies
Social Movement Action Framework
Building momentum for change for BPSO OHT champions at Humber River Hospital
Humber River Hospital is a designated Best Practice Spotlight Organization® (BPSO®) and is also a part of the North Western Toronto BPSO Ontario Health Team (BPSO OHT). During the pandemic, they faced challenges keeping their champions motivated and engaged in their change initiatives. To re-energize their champions, they integrated multiple strategies including building momentum. Read more in this case study.

Humber River Hospital (HRH) (Home - Humber River Hospital (hrh.ca)) (now Humber River Health) is a designated Best Practice Spotlight Organization® (BPSO®) and is also a part of the North Western Toronto BPSO Ontario Health Team (BPSO OHT). During the pandemic, they faced challenges keeping their champions motivated and engaged in their change initiatives. To re-energize their champions, they integrated two key characteristics from the Social Movement Action (SMA) Framework:” Momentum” and “Public Visibility.”
The HRH change team built momentum for change and raised awareness about the BPSO OHT and its work by:
Offering monthly workshops to re-energize and re-engage their champions. Workshop topics included simulation learning and reviewing updated assessments on BPG implementation.
- Producing and sharing a regular newsletter which included BPG implementation tips and updates.
- Giving a “BPSO champion t-shirt” to all champions after completing the workshop.
- Including a QR code in each newsletter and on each BPSO champion t-shirt, linking anyone who scanned the code to a video promoting the BPSO program (see image of t-shirts below.)
As a result of their individual and collective actions, HRH has been able to maintain its champion network. We’re pleased to report that 25 per cent of the nurses in their organization are now trained champions!

Turquoise and Yellow Illustrative Character Project Report Video (canva.com)

Shared with permission from Humber River Hospital as part of the North Western Toronto Best Practice Spotlight Organization® (BPSO®) Ontario Health Team (OHT)

Increasing visibility to advance the rights of Deaf children
A community coalition in Los Angeles, California took collective action to advocate for the rights of Deaf children in accessing child abuse prevention and treatment services. he coalition took multiple steps to increase visibility, spread awareness and gain support. Read more in this case study.
A community coalition in Los Angeles, California took collective action to advocate for the rights of Deaf children in accessing child abuse prevention and treatment services. The coalition took multiple steps to increase visibility, spread awareness and gain support. Some examples:
- one of the member organizations wrote an article published in a magazine for the Deaf community advocating for the protection of Deaf children.
- A presentation by coalition members was made at a local synagogue that included members of the Deaf community.
- A local social event included a focus on the collective actions of the coalition and how attendees could financially support their efforts.
These activities drew further attention to the collective action being taken and the urgency for change (Embry and Grossman, 2006).

Using communication platforms to mobilize change for persons with diabetic foot ulcers
The collective actions of RNAO, Wound Care Canada and other supporters used public visibility strategies to advocate for diabetes-related foot ulcers care. Read more in this case study.
In 2014, RNAO, Wound Care Canada, and other supporters organized a coalition and advocated for diabetes-related foot ulcers care from the provincial government in Ontario, Canada. The coalition used evidence, political pressure to demand an integrated system of care with universal access to improve health outcomes, including reduced ulcers and amputations and reduced costs for pressure-alleviating devices. Members of the coalition participated in many activities, including:
- attending and participating in stakeholder meetings
- writing a media release and lead article in RNJ
- meeting with members of provincial parliament (MPPs) at RNAO’s annual Queen’s Park Day (Grinspun et al., 2018a)
The result of these advocacy efforts and changes in health outcomes are also described in an RNAO Evidence Booster measuring the impact of offloading devices for people living with diabetes and foot ulcers (https://rnao.ca/bpg/resources/evidence-booster-assessment-and-management-foot-ulcers-people-diabetes).

Knowledge-to-Action Framework
Sustaining the Assessment and Management of Pain Best Practice Guideline across a multi-site long-term care home
The Region of Peel, a Best Practice Spotlight Organization® (BPSO®), has sustained the implementation of the Assessment and Management of Pain best practice guideline (BPG) for almost a decade.
The Region of Peel, an RNAO Best Practice Spotlight Organization® (BPSO®) started implementing the RNAO Assessment and Management of Pain best practice guideline (BPG) in 2014 and has sustained its use since then. For example, in their 2019 BPSO annual report, they cited a continuous downward trend in the number of clients who reported a worsening of their pain. Pain experienced by the residents was better controlled, and the staff was found to assess, identify, and manage pain better by using the BPG.
Their keys to success include:
- building on what works (for example, existing practices and policies)
- empowering champions and growing their champion network
- involving residents and families
- gaining support from leaders and partners including RNAO, Peel of Region Leadership, Health Quality Ontario).
- collaborating with an interdisciplinary team
- conducting a formal sustainability evaluation
To learn more about The Region of Peel’s journey in sustaining the use of the Assessing and Managing Pain BPG, along with other BPGs, check out this webinar.

Engaging Persons with Lived Experiences
Holland Bloorview Kids Rehabilitation Hospital: Co-designing change through the active engagement of persons with lived experience
A case study from Holland Bloorview Kids Rehabilitation Hospital focused on engaging persons with lived experience in a change process.
Holland Bloorview Kids Rehabilitation Hospital (hereafter referred to as Holland Bloorview) is a designated Best Practice Spotlight Organization® (BPSO®) in Toronto, Ontario, Canada. Holland Bloorview has an award-winning Family Leadership Program (FLP), through which family leaders partner with the organization and the Bloorview Research Institute to co-design, shape, and improve services, programs, and policies. Family leaders are families and caregivers who have received services at Holland Bloorview, and have lived experiences of paediatric disability. Family leaders’ roles include being a mentor to other families, an advisor to committees and working groups, and faculty who co-teach workshops to students and other families.
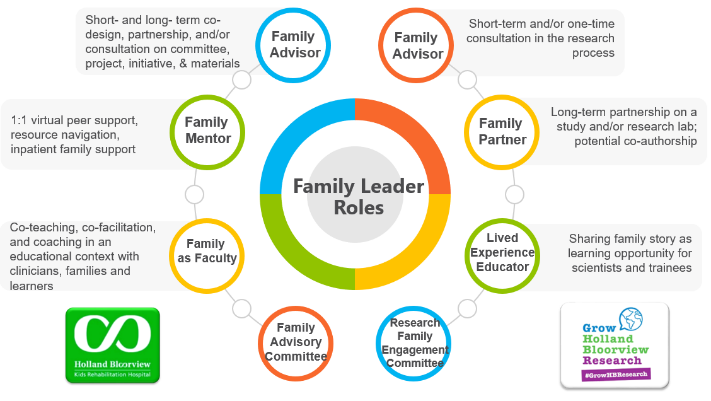
Family Leader Roles at Holland Bloorview. Photo provided with permission by Holland Bloorview Kids Rehabilitation Hospital.
The ENFit™ Working Group is an example of a successful implementation co-design process within Holland Bloorview. The ENFit™ Working Group is an interprofessional team working on the adoption of a new type of connection on products used for enteral feeding [feeding directly through the stomach or intestine via a tube]. By introducing the ENFit™ system, a best practice safety standard, the working group plans to reduce the risk of disconnecting the feeding tube from other medical tubes, and thus decrease harm to children and youth who require enteral feeding.
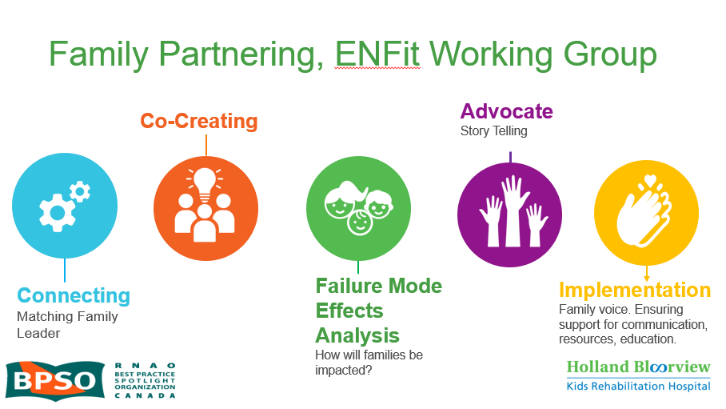
Family Partnering with the EnFit Working Group. Photo provided with permission by Holland Bloorview Kids Rehabilitation Hospital.
The working group invited a family member and leader whose son had received services at Holland Bloorview. This family member had significant lived experience with enteral feeding management, enteral medication administration, and other complexities associated with enteral products. During the meetings, great attention was given to the potential impacts on persons and families. The group engaged the family member by:
- co-creating the implementation plan
- involving them in a failure mode affects analysis, which highlighted the impact of the feeding tube supplies on transitions to home, school, and other care settings
- working with the family member to advocate for safe transitions within the provincial pediatric system, which led to the development of the Ontario Pediatric ENFit™ Group
To learn more about Holland Bloorview’s experience in partnering with families in a co-design process, watch their 38-minute webinar: The Power of Family Partnerships.

