Case studies
Social Movement Action Framework
Transforming long-term care reform
The urgent need to transform long-term care (LTC) in Ontario gained broad support in 2020 during the COVID-19 pandemic. Read more in this case study.
The urgent need to transform long-term care (LTC) in Ontario gained broad support in 2020 during the COVID-19 pandemic. The pandemic exposed long-standing system failings. Examples of triggers included:
- an alarming mortality rate resulting from COVID-19 in LTC settings, representing a large majority of COVID-19-related deaths in Ontario
- a scathing report from the Canadian Armed Forces
- devastating stories from families who were separated from loved ones

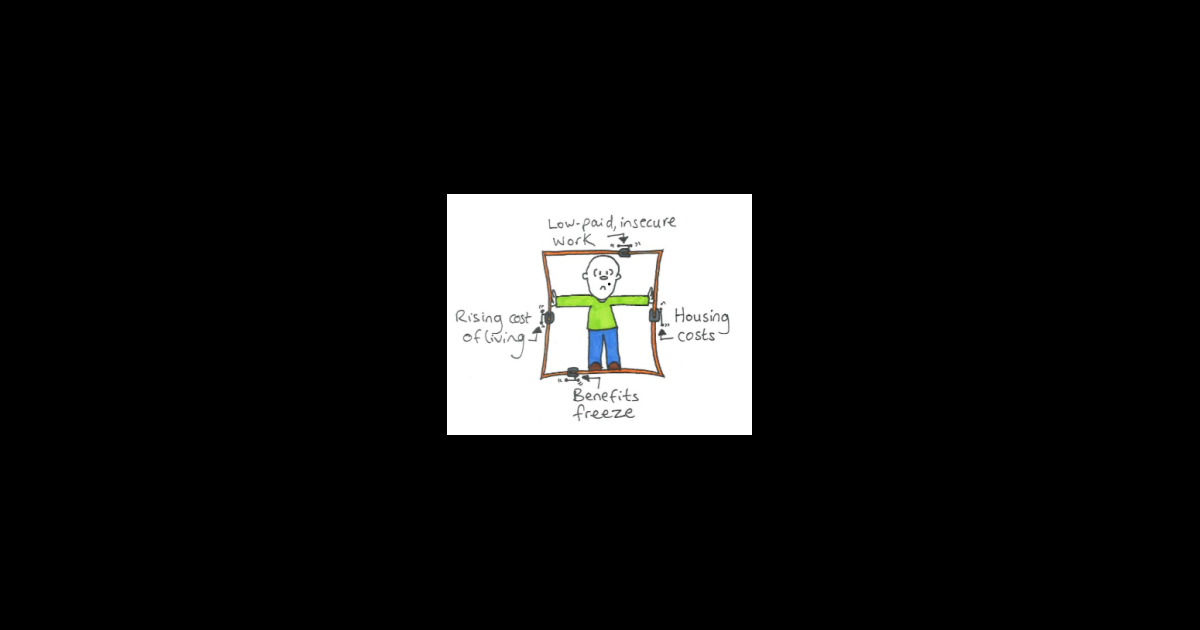
Doodling to frame the issue of poverty
Doodles are a creative expression of framing to position an issue and build meaning. Learn morew in this case study.
Here is an example of a doodle used to frame the issue of poverty. The notion of people being "locked in" by circumstances outside their control is a powerful metaphor. This doodle shows some of the main factors that combine to restrict and restrain people, locking them into poverty. (Joseph Roundtree Foundation)
Engaging champions' narratives
This RNAO champions training program used storytelling, metaphors, collective artwork and personal narratives to frame the importance of person-and family-centred care. Learn more
This RNAO champions training program used storytelling, metaphors, collective artwork and personal narratives to frame the importance of person-and family-centred care.
Knowledge-to-Action Framework
Overcoming barriers to evidence-based practice – Lessons learned from DongZhiMen Hospital and Beijing University of Chinese Medicine (BUCM) School of Nursing
DongZhiMen Hospital and Beijing University of Chinese Medicine (BUCM) School of Nursing are international BPSOs in Beijing, China. Staff at the sites identified barriers to the use of evidence in practice including heavy workloads, cultural differences and reluctant attitudes about using evidence to inform practice.
DongZhiMen Hospital and Beijing University of Chinese Medicine (BUCM) School of Nursing are international BPSOs in Beijing, China. They identified barriers to the use of evidence in practice including heavy workloads, cultural differences and reluctant attitudes about using evidence to inform practice. The assessment and identification of barriers allowed change teams to develop effective strategies for implementation with the input of stakeholders.
For example, for the implementation of the RNAO best practice guideline Assessment and management of foot ulcers for people with diabetes, barriers included
- nursing shortages across China,
- a lack of training to support the development of knowledge and skills in evidence-based nursing practice,
- the costs of guideline implementation. and
- practice recommendations that exceeded local nursing scope.
SOURCE: Transforming Nursing Through Knowledge, 2018.

Evaluating the impact of implementing the Person- and Family-Centred Care Best Practice Guideline at Spectrum Health Care
Spectrum Health Care, a Best Practice Spotlight Organization® (BPSO®) and home health organization, evaluated care outcomes after implementing the Person- and Family-Centred best practice guideline (BPG).
Spectrum Health Care (Spectrum), an RNAO Best Practice Spotlight Organization® (BPSO®), is a home health organization with more than 200 nursing staff across three locations in the province of Ontario, Canada.
Spectrum chose to implement the 2015 Person- and Family-Centred Care (PFCC) Best Practice Guideline (BPG) to enhance person- and family-centred care and to reduce complaints regarding care. Members of the senior leadership team at Spectrum Health Care led implementation together with Spectrum’s Patient and Family Advisory Council.
To support the practice change, Spectrum used the following implementation interventions:
- Conducting a gap analysis to determine the knowledge/practice gap;
- Holding education sessions for staff on person- and family-centred care best practices;
- Revising their care processes to include review of care plans with the person and/or members of their family
- Surveying staff members on their attitudes about person- and family-centred care via surveys
- Developing staff education on communication strategies to support the assessment of a person’s care needs and care plans.
After implementing these interventions, Spectrum assessed the number of complaints received from persons receiving care per 1,000 care visits and compared that to their baseline.
They found a decrease of 42 per cent of complaints from persons received over an 18-month time period at one of the sites that was implementing the PFCC BPG at Spectrum Health Care.
At another site, an 80 per cent reduction in complaints was found following the staff education intervention.
Data analyses overall indicated that the implementation of the PFCC BPG was highly successful in reducing persons' complaints regarding care.
Read more about Spectrum Health care’s results of implementing the PFCC BPG here: Slide 2 (rnao.ca)

Sustaining the Assessment and Management of Pain Best Practice Guideline across a multi-site long-term care home
The Region of Peel, a Best Practice Spotlight Organization® (BPSO®), has sustained the implementation of the Assessment and Management of Pain best practice guideline (BPG) for almost a decade.
The Region of Peel, an RNAO Best Practice Spotlight Organization® (BPSO®) started implementing the RNAO Assessment and Management of Pain best practice guideline (BPG) in 2014 and has sustained its use since then. For example, in their 2019 BPSO annual report, they cited a continuous downward trend in the number of clients who reported a worsening of their pain. Pain experienced by the residents was better controlled, and the staff was found to assess, identify, and manage pain better by using the BPG.
Their keys to success include:
- building on what works (for example, existing practices and policies)
- empowering champions and growing their champion network
- involving residents and families
- gaining support from leaders and partners including RNAO, Peel of Region Leadership, Health Quality Ontario).
- collaborating with an interdisciplinary team
- conducting a formal sustainability evaluation
To learn more about The Region of Peel’s journey in sustaining the use of the Assessing and Managing Pain BPG, along with other BPGs, check out this webinar.
Engaging Persons with Lived Experiences
Integrating patient partners in change – Lessons learned from Kidney Health Australia
Kidnney Health Australia case study
In early 2018, Kidney Health Australia (KHA) developed a guideline for managing percutaneous renal biopsies for individuals with chronic kidney disease (Scholes-Robertson et al., 2019). KHA included 40 persons from across Australia with lived experience of chronic kidney disease and their caregivers – “patient partners”. KHA asked patient partners to prioritize which topics were most important to them during a percutaneous renal biopsy.
Patient partners valued: minimizing discomfort and disruption, protecting their kidneys, enabling self-management, and making sure that support for families and caregivers would be available. They indicated that all of this would help alleviate anxiety and avoid undue stress. Their voices were heard, and KHA effectively incorporated these suggestions in guideline development.
Notably, there were marked differences between the priorities identified by the content experts on the guideline development working group, versus what the patient partners perceived to be important to their health and wellbeing, as shown in the table below.
|
Topics prioritized by content experts |
Topics prioritized by patient partners |
|
|

