Case studies
Social Movement Action Framework
Transforming long-term care reform
The urgent need to transform long-term care (LTC) in Ontario gained broad support in 2020 during the COVID-19 pandemic. Read more in this case study.
The urgent need to transform long-term care (LTC) in Ontario gained broad support in 2020 during the COVID-19 pandemic. The pandemic exposed long-standing system failings. Examples of triggers included:
- an alarming mortality rate resulting from COVID-19 in LTC settings, representing a large majority of COVID-19-related deaths in Ontario
- a scathing report from the Canadian Armed Forces
- devastating stories from families who were separated from loved ones

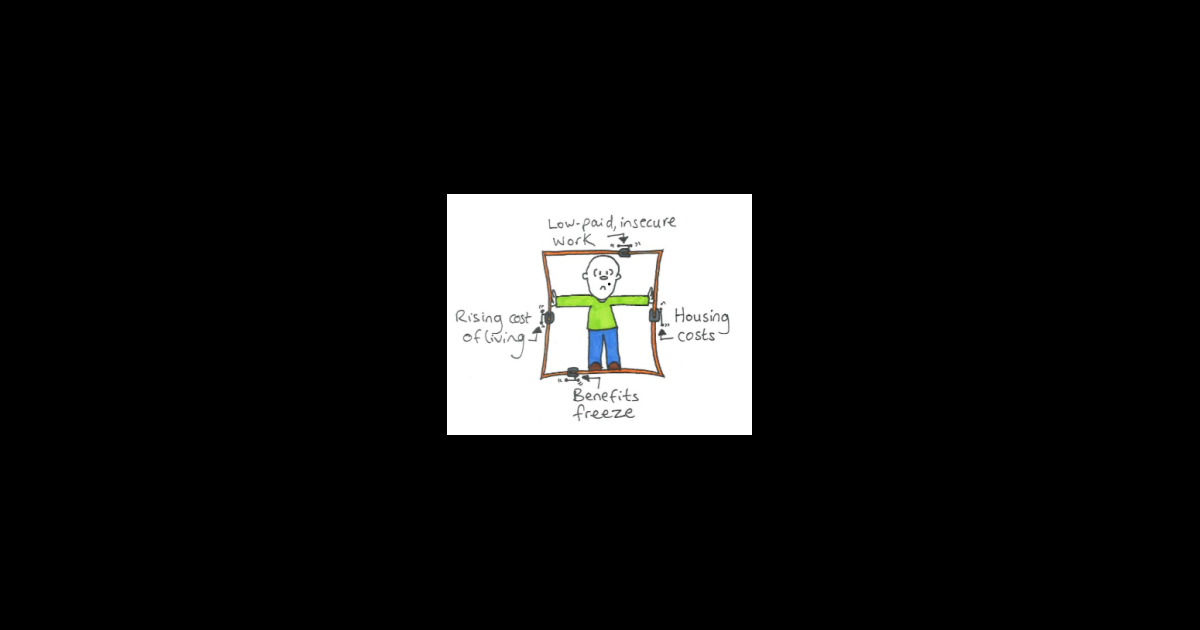
Doodling to frame the issue of poverty
Doodles are a creative expression of framing to position an issue and build meaning. Learn morew in this case study.
Here is an example of a doodle used to frame the issue of poverty. The notion of people being "locked in" by circumstances outside their control is a powerful metaphor. This doodle shows some of the main factors that combine to restrict and restrain people, locking them into poverty. (Joseph Roundtree Foundation)
Engaging champions' narratives
This RNAO champions training program used storytelling, metaphors, collective artwork and personal narratives to frame the importance of person-and family-centred care. Learn more
This RNAO champions training program used storytelling, metaphors, collective artwork and personal narratives to frame the importance of person-and family-centred care.

Knowledge-to-Action Framework
Adapting BPG recommendations to a public health context – Insights from Toronto Public Health
Toronto Public Health – a Best Practice Spotlight Organization® (BPSO®) - has adapted several RNAO best practice guidelines (BPGs) to align with a population health approach.
Toronto Public Health – a Best Practice Spotlight Organization® (BPSO®) in Toronto, Canada – has implemented several RNAO best practice guidelines (BPGs), including Woman Abuse: Screening, Identification and Initial Response (2005) and Preventing and Addressing Abuse and Neglect of Older Adults (2014). Because some practice recommendations in these guidelines focus on the individual person or patient level, they didn’t always align with Toronto Public Health’s population health approach.
To adapt recommendations to the public health context, the change team completed a literature review to explore definitions and adapt strategies to align with the model of care delivery and health promotion philosophy.
Another approach that was taken by Toronto Public Health: piloting BPG recommendations within one small program team. The team would then evaluate the implementation until successful, consistent with the Plan-Do-Study-Act approach). Once successful, the intervention was scaled up within the organization to other programs and teams (Timmings et al., 2018).

Adapting BPG recommendations to a Chinese acute care context to reform care delivery– lessons learned from DongZhiMen Hospital
Care practices were revised using adapted evidence-based best practice guidelines in an acute care facility in Beijing, China.
DongZhiMen Hospital – a BPSO in Beijing China – was motivated to reform care delivery through the use of RNAO BPGs. While best practice recommendations provided general guidance, DongZhimen Hospital identified the need to translate these statements into detailed instructions and parameters tailored to their specific hospital context.
To adapt statements to their context, they translated the guideline into Chinese. A multidisciplinary team then worked through the initial steps of the Knowledge-to-Action Framework. This involved:
- reviewing carefully the evidence to thoroughly understand the intent of the recommendations
- conducting a comprehensive gap analysis
- interviewing staff members and others to identify facilitators and barriers to the use of the BPG.
Using this information, the team was able to create specific, clinical nursing practice standards derived from the recommendations and relevant to their context (Hailing and Runxi, 2018).

Facilitating an evidence-based culture at Unity Health Toronto - St. Michael’s Hospital
Unity Health Toronto - St. Michael’s Hospital, a Best Practice Spotlight Organization® (BPSO®) has embedded evidence-based practices into its culture and daily work processes as part of its corporate strategy.
Unity Health Toronto - St. Michael’s Hospital, a Best Practice Spotlight Organization® (BPSO®) in Toronto, Canada, has embedded evidence-based practices into its culture and daily work processes. Evidence-based practice is part of the hospital’s corporate strategy. It has invested resources to build a critical mass (over 30 per cent) of staff members who are best practice champions.
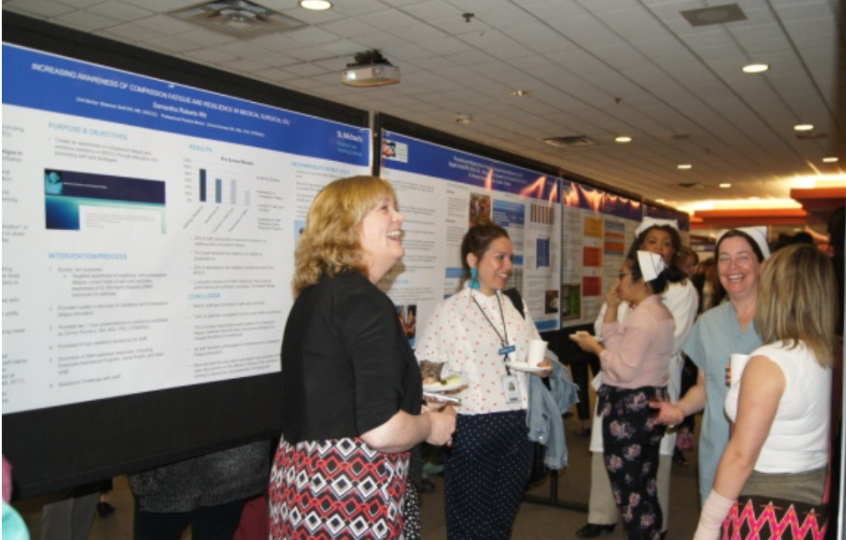
The hospital also provides multiple capacity-building opportunities, including a community of practice, boot camps, booster sessions and mentorship. The annual Nursing Week Gallery Walk, depicted in the image above, is just one way that St. Michael’s Hospital profiles the work of champions and others dedicated to using evidence to inform change initiatives.
SOURCE: Transforming Nursing Through Knowledge, 2018.

Engaging Persons with Lived Experiences
Integrating patient partners in change – Lessons learned from Kidney Health Australia
Kidnney Health Australia case study
In early 2018, Kidney Health Australia (KHA) developed a guideline for managing percutaneous renal biopsies for individuals with chronic kidney disease (Scholes-Robertson et al., 2019). KHA included 40 persons from across Australia with lived experience of chronic kidney disease and their caregivers – “patient partners”. KHA asked patient partners to prioritize which topics were most important to them during a percutaneous renal biopsy.
Patient partners valued: minimizing discomfort and disruption, protecting their kidneys, enabling self-management, and making sure that support for families and caregivers would be available. They indicated that all of this would help alleviate anxiety and avoid undue stress. Their voices were heard, and KHA effectively incorporated these suggestions in guideline development.
Notably, there were marked differences between the priorities identified by the content experts on the guideline development working group, versus what the patient partners perceived to be important to their health and wellbeing, as shown in the table below.
|
Topics prioritized by content experts |
Topics prioritized by patient partners |
|
|

