Case studies
Social Movement Action Framework
Transforming long-term care reform
The urgent need to transform long-term care (LTC) in Ontario gained broad support in 2020 during the COVID-19 pandemic. Read more in this case study.
The urgent need to transform long-term care (LTC) in Ontario gained broad support in 2020 during the COVID-19 pandemic. The pandemic exposed long-standing system failings. Examples of triggers included:
- an alarming mortality rate resulting from COVID-19 in LTC settings, representing a large majority of COVID-19-related deaths in Ontario
- a scathing report from the Canadian Armed Forces
- devastating stories from families who were separated from loved ones

Doodling to frame the issue of poverty
Doodles are a creative expression of framing to position an issue and build meaning. Learn morew in this case study.
Here is an example of a doodle used to frame the issue of poverty. The notion of people being "locked in" by circumstances outside their control is a powerful metaphor. This doodle shows some of the main factors that combine to restrict and restrain people, locking them into poverty. (Joseph Roundtree Foundation)
Engaging champions' narratives
This RNAO champions training program used storytelling, metaphors, collective artwork and personal narratives to frame the importance of person-and family-centred care. Learn more
This RNAO champions training program used storytelling, metaphors, collective artwork and personal narratives to frame the importance of person-and family-centred care.

Knowledge-to-Action Framework
Identifying the problem at Cardioinfantil Foundation of Cardiology Institute (FCI-IC) to achieve excellence in care
Cardioinfantil Foundation of Cardiology Institute is an acute care facility with a goal of achieving excellence in care in the prioritized areas of fall prevention and wound care.
Cardioinfantil Foundation of Cardiology Institute (FCI-IC) is a 340-bed hospital in Bogotá, Colombia. Recognizing that the use of best practice guidelines (BPG) for nursing care was uncommon in Colombia, they joined RNAO’s Best Practice Spotlight Organization® (BPSO®) program with the goal of achieving excellence in care.
FCI-IC had 10 years of evaluation data that revealed problems in specific clinical areas such as fall prevention and wound care. They conducted a baseline diagnostic evaluation to identify the highest priority problems to tackle and to select the most appropriate guidelines and best practice recommendations. As part of this, they surveyed their key partners in the change to learn more about their use of assessment tools, the status of electronic medical records, routine clinical practices such as the use of bed rails, and prevalence data.
This assessment process led to them selecting three RNAO BPGs as knowledge tools: Prevention of Falls and Fall Injuries in the Older Adult, Risk Assessment and Prevention of Pressure Ulcers, and Assessment and Management of Foot Ulcers for People with Diabetes.

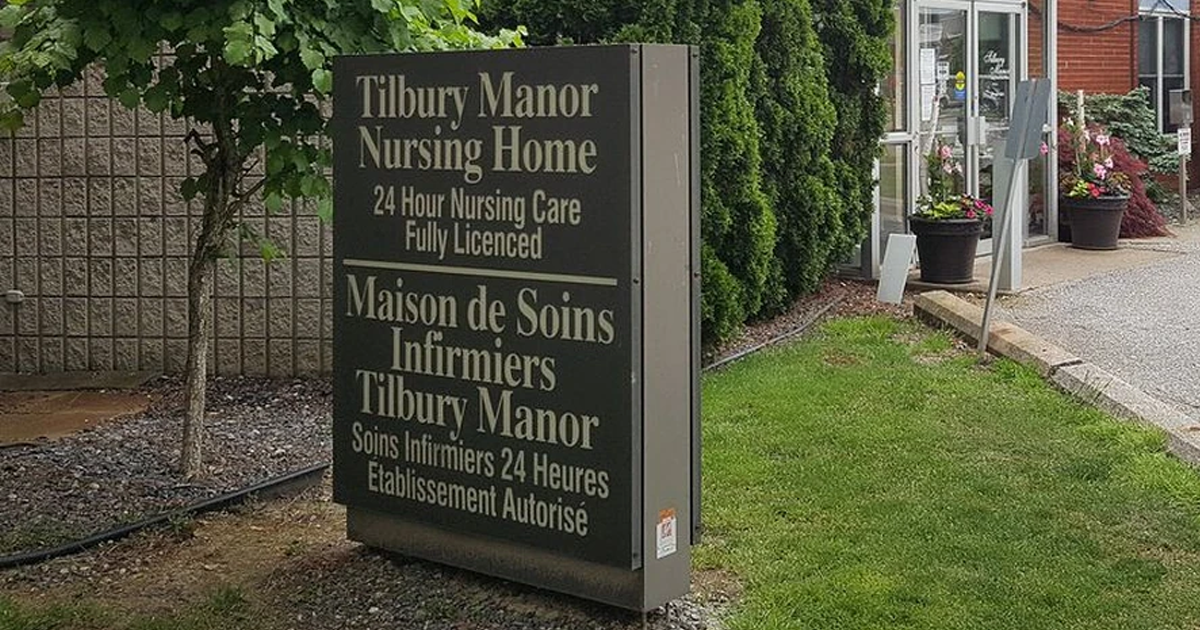
Conducting gap analyses to successfully implement new clinical practices at Tilbury Manor
Tilbury Manor, a long-term care home, chose to focus on provincially-mandated “required programs” when seeking to improve resident care using a gap analysis.
Tilbury Manor, a 75-resident long-term care home in Tilbury chose to focus on provincially-mandated “required programs” (fall prevention, skin and wound care, continence care, bowel management and pain management) when seeking to improve resident care.
They conducted a gap analysis to compare their current practices with the best practices outlined in related RNAO best practice guidelines. Their analysis included an assessment of clinical practices, policies and documentation systems. The results of the gap analysis helped them create specific action plans.
Tilbury Manor then formed project teams led by nurses and supported by a team of champions. These teams proceeded to educate staff, implement new clinical practices, conduct care reviews and conduct audits.
Multiple positive outcomes were reported as a result of implementing these best practices including reductions in reports of pain, less use of restraints, and less falls, pressure ulcers and urinary tract infections.
Adapting the Person- and Family-Centred Care best practice guideline to local context at Sioux Lookout Meno Ya Win Health Centre
Sioux Lookout Meno Ya Win Health Centre (SLMHC) is a pre-designate Best Practice Spotlight Organization® (BPSO®) in Sioux Lookout, a town in Northwestern Ontario. The service area is remote, isolated and encompasses 385,000 square kilometres, with a population that is 85 per cent First Nations. Learn more how this site adapted guidelines to their local context in this case study.
Sioux Lookout Meno Ya Win Health Centre (SLMHC) is a pre-designate Best Practice Spotlight Organization® (BPSO®) in Sioux Lookout, a town in Northwestern Ontario. SLMHC is a hub for inpatient and outpatient hospital services, providing services to including Sioux Lookout and 28 northern communities. The service area is remote, isolated and encompasses 385,000 square kilometres, with a population that is 85 per cent First Nations.
As part of its pre-designation process, the SLMHC change team implemented the Person- and Family- Centred Care (PFCC) best practice guideline (BPG). During implementation, the SLMHC change team worked to adapt the PFCC BPG to the local context of their organization in order to best serve the needs of the population in the surrounding areas as well as in other remote communities.
The SLMCH local context posed unique challenges. Among these:
- Standard guidance on privacy did not always apply to members of the First Nations communities served. Some members wished to have their health information shared with their chief and community.
- Some people must travel as far as 400 or 500 kilometers to return home after discharge from SLMHC. Thus, it was essential to arrange appropriate care transitions and make sure people being discharged would not lose personal belongings.
The SLMHC change team adapted the PFCC BPG to the local context by:
SLMHC Patient Oriented Discharge Summary. Shared with permission.
- placing names on the doors of the hospital rooms of some individuals, so their community members could stop by and visit.
- creating a Patient Oriented Discharge Summary (PODS) that included the following options to indicate the person’s preferences regarding sharing their health information:
- I agree to my health information being shared with________
- I do not agree with my health information being disclosed to people in my community (for example, band or council)
- creating a detailed staff checklist within the PODS to ensure safe care transitions (by, for example, faxing the completed form to an external Indigenous Transition Navigator, or listing personal items collected from the room).
- working with an Indigenous Transitions Facilitator, whose roles include conducting follow-up phone calls with the person, patient rounding, and coordinating safe transitions.
After successfully creating a tailored PODS that meets the need of the population they serve, SLMHC has been able to better support person- and family-centred care principles within the organization.
Shared with permission by Sioux Lookout Meno Ya Win Health Centre

Engaging Persons with Lived Experiences
Integrating patient partners in change – Lessons learned from Kidney Health Australia
Kidnney Health Australia case study
In early 2018, Kidney Health Australia (KHA) developed a guideline for managing percutaneous renal biopsies for individuals with chronic kidney disease (Scholes-Robertson et al., 2019). KHA included 40 persons from across Australia with lived experience of chronic kidney disease and their caregivers – “patient partners”. KHA asked patient partners to prioritize which topics were most important to them during a percutaneous renal biopsy.
Patient partners valued: minimizing discomfort and disruption, protecting their kidneys, enabling self-management, and making sure that support for families and caregivers would be available. They indicated that all of this would help alleviate anxiety and avoid undue stress. Their voices were heard, and KHA effectively incorporated these suggestions in guideline development.
Notably, there were marked differences between the priorities identified by the content experts on the guideline development working group, versus what the patient partners perceived to be important to their health and wellbeing, as shown in the table below.
|
Topics prioritized by content experts |
Topics prioritized by patient partners |
|
|

