Case studies
Social Movement Action Framework
Increasing visibility to advance the rights of Deaf children
A community coalition in Los Angeles, California took collective action to advocate for the rights of Deaf children in accessing child abuse prevention and treatment services. he coalition took multiple steps to increase visibility, spread awareness and gain support. Read more in this case study.
A community coalition in Los Angeles, California took collective action to advocate for the rights of Deaf children in accessing child abuse prevention and treatment services. The coalition took multiple steps to increase visibility, spread awareness and gain support. Some examples:
- one of the member organizations wrote an article published in a magazine for the Deaf community advocating for the protection of Deaf children.
- A presentation by coalition members was made at a local synagogue that included members of the Deaf community.
- A local social event included a focus on the collective actions of the coalition and how attendees could financially support their efforts.
These activities drew further attention to the collective action being taken and the urgency for change (Embry and Grossman, 2006).

Using communication platforms to mobilize change for persons with diabetic foot ulcers
The collective actions of RNAO, Wound Care Canada and other supporters used public visibility strategies to advocate for diabetes-related foot ulcers care. Read more in this case study.
In 2014, RNAO, Wound Care Canada, and other supporters organized a coalition and advocated for diabetes-related foot ulcers care from the provincial government in Ontario, Canada. The coalition used evidence, political pressure to demand an integrated system of care with universal access to improve health outcomes, including reduced ulcers and amputations and reduced costs for pressure-alleviating devices. Members of the coalition participated in many activities, including:
- attending and participating in stakeholder meetings
- writing a media release and lead article in RNJ
- meeting with members of provincial parliament (MPPs) at RNAO’s annual Queen’s Park Day (Grinspun et al., 2018a)
The result of these advocacy efforts and changes in health outcomes are also described in an RNAO Evidence Booster measuring the impact of offloading devices for people living with diabetes and foot ulcers (https://rnao.ca/bpg/resources/evidence-booster-assessment-and-management-foot-ulcers-people-diabetes).

Using social media to increase public visibility and raise awareness
Social media is used by RNAO regularly to advocate for advancing the rights of Ontarians, including residents of long-term care homes. Read this case study that includes examples of effective social media campaigns advocating for the Nursing home Basic Care Guarantee.
RNAO uses social media campaigns to increase public visibility and raise awareness of issues. One example: RNAO’s call on the Ontario government to mandate recommendations set out in its Nursing Home Basic Care Guarantee. The campaign incorporated the hashtags #LTC #BasicCareGuarantee and #4Hours4Seniors to raise awareness of the staffing crisis in long-term care (LTC) and to encourage the public, health professionals, the government, LTC residents and their families to mobilize change.
As the campaign evolved, so did the visuals and the messaging. The three examples below show the stages of the campaign as it gained attention and momentum – from “good” through “better” to “best.”
RNAO developed an Action Alert (AA) to mobilize collective action to advocate for nursing home residents. The link to the AA, the graphic, the messaging and the hashtag #4Hours4Seniors were all shared on social media to urge others to sign and share the AA. People were also encouraged to use the hashtag to contribute to the dialogue about the LTC crisis.
The social media campaign aimed to support the goal set out in the AA – encourage as many people as possible to add their signatures to urge action from key political leaders.
This is a good example of a social media campaign, incorporating a graphic, supportive messaging, a call-to-action (the link to the AA) and a specific hashtag.
In this example, RNAO staff members are holding signs identifying why #4Hours4Seniors matters to them. The hashtag is used consistently and individual reasons for supporting the cause are illustrated.
This is a better example of a social media campaign – it brings a personal touch to the campaign and allows supporters to share why they want to join the conversation. It also brought life to the hashtag and to the purpose of the campaign.
Image
In this example, RNAO collaborated with F.J. Davey Home in Sudbury, Ontario, Canada to encourage residents to share their “why” for wanting #4Hours4Seniors. Building on the same idea as the “better” example given above, this example truly brought a face to the reason for the campaign in the first place. RNAO shared the photos and quotes from residents on its social media feeds (Instagram, Facebook and Twitter) alongside the hashtag #4Hours4Seniors.
For example, M. Doan, a senior living at the F.J. Davey Home, shared: “I am a very independent person, but my wife on the other hand isn’t and she means the world to me. With four hours of care, it doesn’t need to be rushed. And who wouldn’t want to see her beautiful smile for four hours!" (https://twitter.com/RNAO/status/1336781022780928000).
The photos are powerful as they show a real-life married couple living in a LTC home – two of the many residents RNAO advocated for through its AA and its ongoing call for a Nursing Home Basic Care Guarantee. The posters held by the couple express their personal values of dignity and comfort.
Knowledge-to-Action Framework
Identifying the problem at Cardioinfantil Foundation of Cardiology Institute (FCI-IC) to achieve excellence in care
Cardioinfantil Foundation of Cardiology Institute is an acute care facility with a goal of achieving excellence in care in the prioritized areas of fall prevention and wound care.
Cardioinfantil Foundation of Cardiology Institute (FCI-IC) is a 340-bed hospital in Bogotá, Colombia. Recognizing that the use of best practice guidelines (BPG) for nursing care was uncommon in Colombia, they joined RNAO’s Best Practice Spotlight Organization® (BPSO®) program with the goal of achieving excellence in care.
FCI-IC had 10 years of evaluation data that revealed problems in specific clinical areas such as fall prevention and wound care. They conducted a baseline diagnostic evaluation to identify the highest priority problems to tackle and to select the most appropriate guidelines and best practice recommendations. As part of this, they surveyed their key partners in the change to learn more about their use of assessment tools, the status of electronic medical records, routine clinical practices such as the use of bed rails, and prevalence data.
This assessment process led to them selecting three RNAO BPGs as knowledge tools: Prevention of Falls and Fall Injuries in the Older Adult, Risk Assessment and Prevention of Pressure Ulcers, and Assessment and Management of Foot Ulcers for People with Diabetes.

Conducting gap analyses to successfully implement new clinical practices at Tilbury Manor
Tilbury Manor, a long-term care home, chose to focus on provincially-mandated “required programs” when seeking to improve resident care using a gap analysis.
Tilbury Manor, a 75-resident long-term care home in Tilbury chose to focus on provincially-mandated “required programs” (fall prevention, skin and wound care, continence care, bowel management and pain management) when seeking to improve resident care.
They conducted a gap analysis to compare their current practices with the best practices outlined in related RNAO best practice guidelines. Their analysis included an assessment of clinical practices, policies and documentation systems. The results of the gap analysis helped them create specific action plans.
Tilbury Manor then formed project teams led by nurses and supported by a team of champions. These teams proceeded to educate staff, implement new clinical practices, conduct care reviews and conduct audits.
Multiple positive outcomes were reported as a result of implementing these best practices including reductions in reports of pain, less use of restraints, and less falls, pressure ulcers and urinary tract infections.
Adapting the Person- and Family-Centred Care best practice guideline to local context at Sioux Lookout Meno Ya Win Health Centre
Sioux Lookout Meno Ya Win Health Centre (SLMHC) is a pre-designate Best Practice Spotlight Organization® (BPSO®) in Sioux Lookout, a town in Northwestern Ontario. The service area is remote, isolated and encompasses 385,000 square kilometres, with a population that is 85 per cent First Nations. Learn more how this site adapted guidelines to their local context in this case study.
Sioux Lookout Meno Ya Win Health Centre (SLMHC) is a pre-designate Best Practice Spotlight Organization® (BPSO®) in Sioux Lookout, a town in Northwestern Ontario. SLMHC is a hub for inpatient and outpatient hospital services, providing services to including Sioux Lookout and 28 northern communities. The service area is remote, isolated and encompasses 385,000 square kilometres, with a population that is 85 per cent First Nations.
As part of its pre-designation process, the SLMHC change team implemented the Person- and Family- Centred Care (PFCC) best practice guideline (BPG). During implementation, the SLMHC change team worked to adapt the PFCC BPG to the local context of their organization in order to best serve the needs of the population in the surrounding areas as well as in other remote communities.
The SLMCH local context posed unique challenges. Among these:
- Standard guidance on privacy did not always apply to members of the First Nations communities served. Some members wished to have their health information shared with their chief and community.
- Some people must travel as far as 400 or 500 kilometers to return home after discharge from SLMHC. Thus, it was essential to arrange appropriate care transitions and make sure people being discharged would not lose personal belongings.
The SLMHC change team adapted the PFCC BPG to the local context by:
SLMHC Patient Oriented Discharge Summary. Shared with permission.
- placing names on the doors of the hospital rooms of some individuals, so their community members could stop by and visit.
- creating a Patient Oriented Discharge Summary (PODS) that included the following options to indicate the person’s preferences regarding sharing their health information:
- I agree to my health information being shared with________
- I do not agree with my health information being disclosed to people in my community (for example, band or council)
- creating a detailed staff checklist within the PODS to ensure safe care transitions (by, for example, faxing the completed form to an external Indigenous Transition Navigator, or listing personal items collected from the room).
- working with an Indigenous Transitions Facilitator, whose roles include conducting follow-up phone calls with the person, patient rounding, and coordinating safe transitions.
After successfully creating a tailored PODS that meets the need of the population they serve, SLMHC has been able to better support person- and family-centred care principles within the organization.
Shared with permission by Sioux Lookout Meno Ya Win Health Centre

Engaging Persons with Lived Experiences
Holland Bloorview Kids Rehabilitation Hospital: Co-designing change through the active engagement of persons with lived experience
A case study from Holland Bloorview Kids Rehabilitation Hospital focused on engaging persons with lived experience in a change process.
Holland Bloorview Kids Rehabilitation Hospital (hereafter referred to as Holland Bloorview) is a designated Best Practice Spotlight Organization® (BPSO®) in Toronto, Ontario, Canada. Holland Bloorview has an award-winning Family Leadership Program (FLP), through which family leaders partner with the organization and the Bloorview Research Institute to co-design, shape, and improve services, programs, and policies. Family leaders are families and caregivers who have received services at Holland Bloorview, and have lived experiences of paediatric disability. Family leaders’ roles include being a mentor to other families, an advisor to committees and working groups, and faculty who co-teach workshops to students and other families.
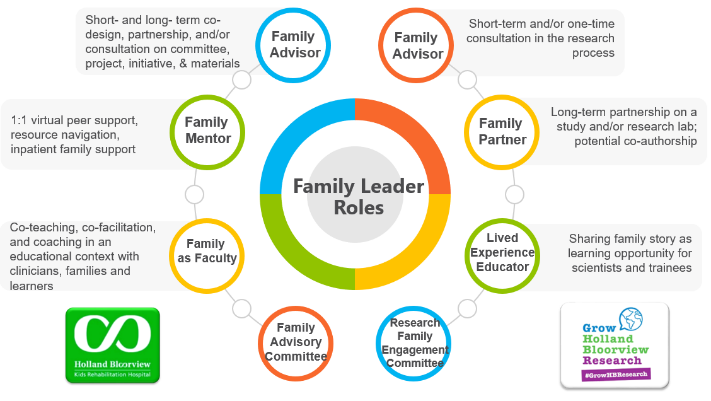
Family Leader Roles at Holland Bloorview. Photo provided with permission by Holland Bloorview Kids Rehabilitation Hospital.
The ENFit™ Working Group is an example of a successful implementation co-design process within Holland Bloorview. The ENFit™ Working Group is an interprofessional team working on the adoption of a new type of connection on products used for enteral feeding [feeding directly through the stomach or intestine via a tube]. By introducing the ENFit™ system, a best practice safety standard, the working group plans to reduce the risk of disconnecting the feeding tube from other medical tubes, and thus decrease harm to children and youth who require enteral feeding.
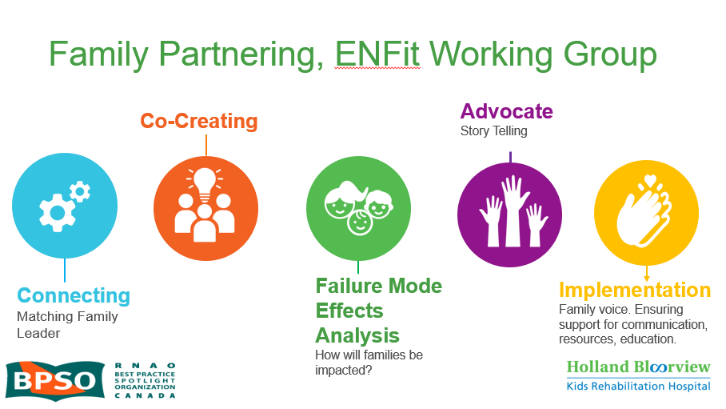
Family Partnering with the EnFit Working Group. Photo provided with permission by Holland Bloorview Kids Rehabilitation Hospital.
The working group invited a family member and leader whose son had received services at Holland Bloorview. This family member had significant lived experience with enteral feeding management, enteral medication administration, and other complexities associated with enteral products. During the meetings, great attention was given to the potential impacts on persons and families. The group engaged the family member by:
- co-creating the implementation plan
- involving them in a failure mode affects analysis, which highlighted the impact of the feeding tube supplies on transitions to home, school, and other care settings
- working with the family member to advocate for safe transitions within the provincial pediatric system, which led to the development of the Ontario Pediatric ENFit™ Group
To learn more about Holland Bloorview’s experience in partnering with families in a co-design process, watch their 38-minute webinar: The Power of Family Partnerships.

Engaging Patient Family Advisors to advance guideline implementation at Scarborough Health Network
A case study about the integration of patient family advisors at Scarborough Health Network to enhance community engagement and health equity.
Scarborough Health Network (SHN) (Home - Scarborough Health Network (shn.ca) is an organization pursuing Best Practice Spotlight Organization® (BPSO®) designation in Scarborough, Ontario, Canada. Patient Family Advisors (PFAs) are a vital part of SHN’s philosophy of care, representing the diverse community SHN serves. A key element of the PFA role is sharing lived experiences with SHN staff and the Scarborough community.
SHN has demonstrated commitment to the role of PFAs within their organization by creating a new department for health equity, patient and community engagement (HEPCE). This department focuses on:
- recruiting, onboarding, managing, recognizing and retaining PFAs
- educating staff on best practices related to engaging with PFAs
During recruitment and onboarding, the HEPCE and current PFAs educate potential PFAs about the role’s scope and expectations. All PFAs are also provided with information on how to share their patient or caregiver story with their audience.
PFAs have played an important role in SHN’s BPSO committee. Indeed, one PFA has been integral to the process of recruiting and engaging champions at SHN throughout the COVID-19 pandemic’s health human resources (HHR) crisis. Their role has included participating in champions’ virtual drop-in sessions (2020-2021) and in-person roadshows (2022).
Champion roadshows are events during, which SHN practice leaders and PFAs promote the BPSO program, share best practice guidelines and recruit champions around the organization, without asking busy staff members to leave their units.
The PFA also supported the recruitment and engagement of champions by:
- collaborating with other champions and working group members to plan champions’ drop-in sessions and roadshows
- working alongside the team to plan safe spaces for staff and PFAs to share their stories
- sharing stories of positive experiences with staff members in relation to the impact of best practices (for example, RNAO’s Person and Family Centred-Care best practice guideline) on their experience
Staff members have reported being motivated to become best practice champions after attending a champion’s roadshow. SHN has also consistently gained champions during the HHR crisis and maintains at least 15 per cent of nursing staff as best practice champions.
The PFA’s role was vital to demonstrating the lasting impact of best practices. They have expressed feeling empowered by their role in BPSO work, expressing that the work helped them find their voice and become part of the movement to promote and implement best practices.
Overall, PFAs play an essential – and dual – role in supporting the implementation of best practices at SHN. In line with person- and family-centred care, PFAs assume an outward-facing role in shaping the implementation of best practices and SHN’s values. In addition, they also act in an inward-facing role to support the bolstering of champions.
To learn more about the PFA role at SHN, please visit the following link: Patient Family Advisors.
Shared with permission by Scarborough Health Network

Co-designing change through the active engagement of persons with lived experience - Holland Bloorview Kids Rehabilitation Hospital
Case study - Holland Bloorview
Holland Bloorview Kids Rehabilitation Hospital (Holland Bloorview) is a designated Best Practice Spotlight Organization® (BPSO®) in Toronto, Canada. Holland Bloorview has an award-winning Family Leadership Program (FLP), through which family leaders partner with the organization and the Bloorview Research Institute to co-design, shape and improve services, programs and policies.
These family leaders are families and caregivers who have received services at Holland Bloorview and have lived experiences of paediatric disability. Their roles include mentoring other families, acting as advisors to committees and working groups, and co-teaching workshops to students and other families.
One example of a successful implementation co-design within Holland Broadview is the ENFit™ Working Group. This interprofessional team works on the adoption of a new type of connection on products used for enteral feeding – or feeding directly through the stomach or intestine via a tube. By introducing the ENFit™ system, a best practice safety standard, the working group plans to reduce the risk of disconnecting the feeding tube from other medical tubes. This in turn decreases harm to children and youth who require enteral feeding.
The working group invited a family member and leader whose son had received services at Holland Bloorview. This family member had significant lived experience with enteral feeding management, enteral medication administration, and other complexities associated with enteral products. During the meetings, the potential impacts on persons and families were emphasized. The working group engaged the family member by:
- co-creating the implementation plan
- involving them in a failure mode and effects analysis highlighting the impact of the feeding tube supplies on transitions to home, school and other care settings
- working with the family member to advocate for safe transitions within the provincial pediatric system, which led to the development of the Ontario Pediatric ENFit™ Group
To learn more about Holland Bloorview’s experience in partnering with families in a co-design process, watch their 38-minute webinar: The Power of Family Partnerships
Shared with permission from Holland Bloorview

