Case studies
Social Movement Action Framework
Engaging an interprofessional change team to lead implementation: West Park Healthcare Centre
West Park Healthcare Centre applied a call to action to implement best practice guidelines with the support and guidance of their senior leadership and implementation teams. Learn more about the role of core leadership structures in this case study.
West Park Healthcare Centre, an RNAO BPSO, is a rehabilitation and complex care centre in Toronto, Canada. They applied a compelling call to action to implement these RNAO BPGs: Assessment and Management of Pain, Client Centred Care and Prevention of Falls and Fall Injuries in the Older Adult.
With support from senior leadership, interprofessional change teams – including nurse leaders, such as advanced practice nurses and nurse practitioners – were responsible for leading the implementation strategies, which included taking collective action. Implementation efforts focused on engaging in quality improvement measures, promoting the culture and values of evidence-based practice and aligning their implementation efforts to the organization’s culture and values.
As members of the implementation teams, the nurse leaders were influencers who aimed to build collaborative and committed relationships amongst the interprofessional team and create a work environment that empowered staff to take evidence-based action. The team embraced diverse perspectives and knowledge to allow for adaptations to the local context.

Engaging collective strength in action at Central West Specialized Developmental Services
The change team at Central West Specialized Developmental Services (CWSDS) has built a strong core leadership structure to support their implementation efforts by including both formal and informal leaders.
Central West Specialized Developmental Services (CWSDS) is a pre-designate Best Practice Spotlight Organization® (BPSO®.) During the BPSO pre-designation process, the CWSDS change team has built a strong core leadership structure to support the implementation of best practices, by including both formal and informal leaders.
The CWSDS change team relied on the following strategies to build a strong core leadership structure:
CWSDS’s RNAO-BPSO organizational structure. Figure provided with permission by CWSDS.
- embedding the RNAO BPSO pre-designation process within the organization’s strategic plan.
- emphasizing the interprofessional nature of the initiative by encouraging professionals from all disciplines to become involved.
- engaging an interprofessional team of stakeholders within the organization with the change, including direct support professionals, managers, food services, human resources staff, and members of the communication and information technology teams.
- encouraging stakeholders to become trained RNAO Best Practice Champions and to participate in RNAO events.
- making sure all stakeholders were informed and involved in the change initiative (by, for example, providing updates during managerial meetings and including stakeholders in completing gap analyses.)
- supporting Best Practice Champions in leading best practice guideline (BPG) implementation alongside the BPSO Steering Committee.
As a result of the change team’s work to build a core leadership structure, they were able to tailor the implementation of BPGs toward daily clinical problems relevant to their direct support professionals. This increased recognition of and support for their change initiative.
To learn more about CWSDS’s BPG implementation journey, watch their 38-minute webinar: Collective Strength in Action: How to Promote and Implement Best Practice Guidelines.
Engaging a network to strengthen alliances for an Indigenous school diabetes prevention project
An Indigenous diabetes prevention school project used a network to support community partner's capacity building and collaboration. Read more in this case study.
In Quebec, Canada, community groups and researchers participated in a network using social movement approaches for the Kahnawake Schools Diabetes Prevention Project. In the early phase of the social movement, the network supported capacity building and collaboration of the community members. As the movement evolved, the network strengthened alliances among the community members and their shared decision-making. It also supported the program’s expansion to more children. At the conclusion of the project, the network supported the emerging leadership of the community partners (Tremblay et al., 2018).

Knowledge-to-Action Framework
Sustaining the Assessment and Management of Pain Best Practice Guideline across a multi-site long-term care home
The Region of Peel, a Best Practice Spotlight Organization® (BPSO®), has sustained the implementation of the Assessment and Management of Pain best practice guideline (BPG) for almost a decade.
The Region of Peel, an RNAO Best Practice Spotlight Organization® (BPSO®) started implementing the RNAO Assessment and Management of Pain best practice guideline (BPG) in 2014 and has sustained its use since then. For example, in their 2019 BPSO annual report, they cited a continuous downward trend in the number of clients who reported a worsening of their pain. Pain experienced by the residents was better controlled, and the staff was found to assess, identify, and manage pain better by using the BPG.
Their keys to success include:
- building on what works (for example, existing practices and policies)
- empowering champions and growing their champion network
- involving residents and families
- gaining support from leaders and partners including RNAO, Peel of Region Leadership, Health Quality Ontario).
- collaborating with an interdisciplinary team
- conducting a formal sustainability evaluation
To learn more about The Region of Peel’s journey in sustaining the use of the Assessing and Managing Pain BPG, along with other BPGs, check out this webinar.

Engaging Persons with Lived Experiences
Holland Bloorview Kids Rehabilitation Hospital: Co-designing change through the active engagement of persons with lived experience
A case study from Holland Bloorview Kids Rehabilitation Hospital focused on engaging persons with lived experience in a change process.
Holland Bloorview Kids Rehabilitation Hospital (hereafter referred to as Holland Bloorview) is a designated Best Practice Spotlight Organization® (BPSO®) in Toronto, Ontario, Canada. Holland Bloorview has an award-winning Family Leadership Program (FLP), through which family leaders partner with the organization and the Bloorview Research Institute to co-design, shape, and improve services, programs, and policies. Family leaders are families and caregivers who have received services at Holland Bloorview, and have lived experiences of paediatric disability. Family leaders’ roles include being a mentor to other families, an advisor to committees and working groups, and faculty who co-teach workshops to students and other families.
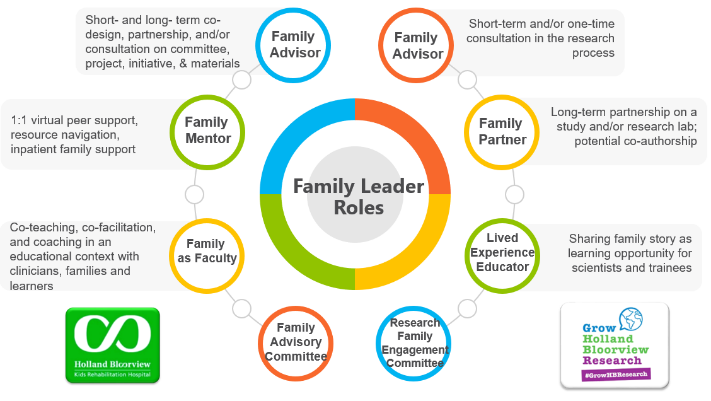
Family Leader Roles at Holland Bloorview. Photo provided with permission by Holland Bloorview Kids Rehabilitation Hospital.
The ENFit™ Working Group is an example of a successful implementation co-design process within Holland Bloorview. The ENFit™ Working Group is an interprofessional team working on the adoption of a new type of connection on products used for enteral feeding [feeding directly through the stomach or intestine via a tube]. By introducing the ENFit™ system, a best practice safety standard, the working group plans to reduce the risk of disconnecting the feeding tube from other medical tubes, and thus decrease harm to children and youth who require enteral feeding.
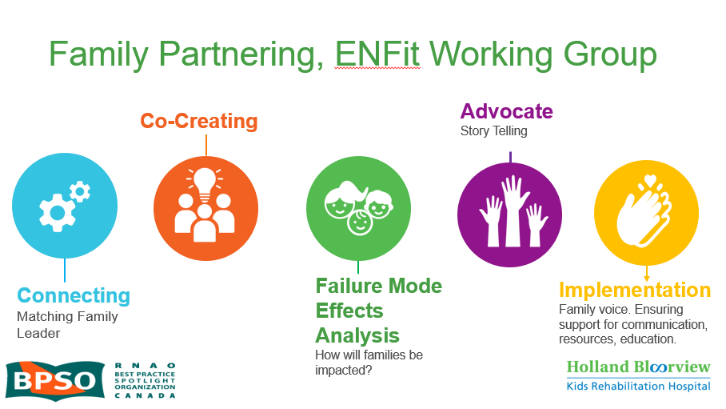
Family Partnering with the EnFit Working Group. Photo provided with permission by Holland Bloorview Kids Rehabilitation Hospital.
The working group invited a family member and leader whose son had received services at Holland Bloorview. This family member had significant lived experience with enteral feeding management, enteral medication administration, and other complexities associated with enteral products. During the meetings, great attention was given to the potential impacts on persons and families. The group engaged the family member by:
- co-creating the implementation plan
- involving them in a failure mode affects analysis, which highlighted the impact of the feeding tube supplies on transitions to home, school, and other care settings
- working with the family member to advocate for safe transitions within the provincial pediatric system, which led to the development of the Ontario Pediatric ENFit™ Group
To learn more about Holland Bloorview’s experience in partnering with families in a co-design process, watch their 38-minute webinar: The Power of Family Partnerships.

