Case studies
Social Movement Action Framework
Scaling up, scaling out and scaling deep a fall prevention initiative
A joint fall prevention program by RNAO and the Canadian Patient Safety Institute (CPSI) that was scaled up, scaled out and scaled deep.
RNAO’s Best Practice Spotlight Organization® (BPSO®) program itself was scaled up, scaled out and scaled deep – on the national level – when RNAO and the Canadian Patient Safety Institute (CPSI) entered into a formal partnership on a pan-Canadian falls prevention initiative campaign in 2007, with a focus on long-term care (LTC) (McConnell et al., 2018).
This collaboration involved the implementation of best practices, capacity building at the micro and meso levels with individuals and organizations, and engagement with national partners. The work was informed by the first and second editions of RNAO’s best practice guideline (BPG) Prevention of Falls and Fall Injuries in the Older Adult and CPSI’s program Safer Healthcare Now! on falls prevention as a critical patient safety issue Reducing Falls and Injuries from Falls.
The National Collaborative on Falls Prevention in Long-Term Care, launched in 2008–2009, included staff from 32 LTC homes and an interprofessional expert panel. The goals of the collaborative:
- to reduce the rate of falls in older adults by educating and training staff and patients about fall prevention
- develop a forum for improvement teams
- participate in a methodology on quality improvement initiatives using the Model for Improvement (Langley et al., 2009).
The collaboration was highly successful – process indicators showed decreased rates of falls in the LTC homes following implementation. However, it was determined that more time and support would be needed to scale the fall prevention initiative out and deep to in order to embed and sustain the practice changes.
In 2010–2011, the collaborative expanded to a national campaign where the program was delivered virtually to more than 45 organizations from diverse health sectors using web-based technology. This enabled greater access to the program with impressive outcomes, and showed that technology could be used as a tool to scale the program up and out.
This was followed up by creation and delivery of a fall prevention learning series in 2011–2012 to strengthen the uptake and sustainability of best practices. The training integrated implementation science, change theory and quality improvement methodology. As with the other collaboration components, the outcomes of the learning series demonstrated improvements in practice changes and reductions in falls causing injury, and organizational policies to support and sustain the change. The continued use of evaluation to determine outcomes and impact as part of quality improvement and using ongoing audit and feedback demonstrated a change that was scaled deep.
The collaboration helped embed principles of social action movement by its focus on a credible and important shared concern – preventing falls – where urgent change was needed. Momentum was used to support the continued engagement of fall prevention champions across sectors. Networks were used to share resources and expand collaborations across communities.

Building capacity in change agents for health innovation and transformation
United Kingdom junior doctors increased their capacity as change agents after mobilizing and implementing the WHO surgical checklist.
Although positioned as the “future leaders of health-care transformation and innovation,” junior doctors (or interns) in the United Kingdom actually receive very little training in leadership competencies at medical schools to prepare for this role (Carson-Steven et al., 2013). Instead, they learn in clinical environments that are frequently unreceptive to change and innovation informed by best practices.
To overcome these barriers and emerge as leaders, a group of junior doctors chose to independently learn how to innovate and champion evidence-based practice by applying social movement approaches including mobilizing for change. By participating in programs, such as the Institute for Healthcare Improvement’s “Open Schools,” they built capacity in social movement thinking and actions and used their knowledge, skills, networks and experiential learning to drive change in their clinical practice.
The junior doctors applied social movement actions when they led a change initiative to implement the World Health Organization’s guidelines on the use of surgical safety checklists for patient safety. They co-created a supportive learning community to learn together and from one another and to overcome obstacles and resistance. As emerging leaders, they engaged in collective action, including organizing a “teach-in” to raise awareness about the urgent need for change and the implementation of best practices in surgical care as determined through evidence. And, each doctor committed to recruiting colleagues to strengthen the social movement and build momentum and a critical mass.
For more details, see The social movement drive: a role for junior doctors in healthcare reform - PubMed (nih.gov).

Championing BPG implementation at Clinica las Condes
at Clínica las Condes (CLC), a Latin American Best Practice Spotlight Organization® (BPSO®) in Santiago, Chile, BP Champions are committed volunteers consisting mostly of nurses and other health professionals. Their leadership is evident in the multiple activities . Learn more in this case study.
The Best Practice Guideline (BPG) Program has supported the leadership and influence of thousands of Registered Nurses’ Association of Ontario (RNAO) Best Practice (BP) Champions as change agents engaged in the implementation of evidence-based practice changes.
For example, at Clínica las Condes (CLC), a Latin American Best Practice Spotlight Organization® (BPSO®) in Santiago, Chile, BP Champions are committed volunteers consisting mostly of nurses and other health professionals. Their leadership is evident in the multiple activities they lead, including:
- reviewing guidelines and organizational policies
- motivating colleagues
- presenting guideline recommendations at clinical services meetings twice a year
- ensuring adherence to practice changes in their clinical units
(Serna Restrepo et al., 2018)

Knowledge-to-Action Framework
Implementing effective interventions for drug and alcohol use using Screening, Brief Intervention and Referral to Treatment (SBIRT)
Evidence-based interventions to support the development of a screening, brief intervention and referral to treatment (SBIRT) for persons who use drugs and alcohol.
Screening, Brief Intervention, and Referral to Treatment (SBIRT) is endorsed by the Substance Abuse and Mental Health Services Administration as an effective intervention for drug and alcohol use. SBIRT has been implemented in multiple health-care settings including acute care.
Implementation leaders were asked to identify barriers, facilitators, as well as implementation strategies that would be most helpful. From this review, implementation leaders perceived that providing ongoing consultation to clinicians for using SBIRT, distributing educational materials to clinicians, and conducting audits and providing feedback were the most helpful.
All implementation leaders voiced the value of available training resources, and peer support as they moved through the implementation process.
Implementation leaders felt more confident leading change in the future due to the knowledge and skills they developed during SBIRT implementation. They also learned the importance of leveraging support from other interprofessional team members, such as social workers and clinical educators.
Read more about it here. Learn more about SBIRT here. Or, review our best practice guideline, Engaging Clients Who Use Substances.

Adapting BPG recommendations to a public health context – Insights from Toronto Public Health
Toronto Public Health – a Best Practice Spotlight Organization® (BPSO®) - has adapted several RNAO best practice guidelines (BPGs) to align with a population health approach.
Toronto Public Health – a Best Practice Spotlight Organization® (BPSO®) in Toronto, Canada – has implemented several RNAO best practice guidelines (BPGs), including Woman Abuse: Screening, Identification and Initial Response (2005) and Preventing and Addressing Abuse and Neglect of Older Adults (2014). Because some practice recommendations in these guidelines focus on the individual person or patient level, they didn’t always align with Toronto Public Health’s population health approach.
To adapt recommendations to the public health context, the change team completed a literature review to explore definitions and adapt strategies to align with the model of care delivery and health promotion philosophy.
Another approach that was taken by Toronto Public Health: piloting BPG recommendations within one small program team. The team would then evaluate the implementation until successful, consistent with the Plan-Do-Study-Act approach). Once successful, the intervention was scaled up within the organization to other programs and teams (Timmings et al., 2018).

Adapting BPG recommendations to a Chinese acute care context to reform care delivery– lessons learned from DongZhiMen Hospital
Care practices were revised using adapted evidence-based best practice guidelines in an acute care facility in Beijing, China.
DongZhiMen Hospital – a BPSO in Beijing China – was motivated to reform care delivery through the use of RNAO BPGs. While best practice recommendations provided general guidance, DongZhimen Hospital identified the need to translate these statements into detailed instructions and parameters tailored to their specific hospital context.
To adapt statements to their context, they translated the guideline into Chinese. A multidisciplinary team then worked through the initial steps of the Knowledge-to-Action Framework. This involved:
- reviewing carefully the evidence to thoroughly understand the intent of the recommendations
- conducting a comprehensive gap analysis
- interviewing staff members and others to identify facilitators and barriers to the use of the BPG.
Using this information, the team was able to create specific, clinical nursing practice standards derived from the recommendations and relevant to their context (Hailing and Runxi, 2018).

Engaging Persons with Lived Experiences
Holland Bloorview Kids Rehabilitation Hospital: Co-designing change through the active engagement of persons with lived experience
A case study from Holland Bloorview Kids Rehabilitation Hospital focused on engaging persons with lived experience in a change process.
Holland Bloorview Kids Rehabilitation Hospital (hereafter referred to as Holland Bloorview) is a designated Best Practice Spotlight Organization® (BPSO®) in Toronto, Ontario, Canada. Holland Bloorview has an award-winning Family Leadership Program (FLP), through which family leaders partner with the organization and the Bloorview Research Institute to co-design, shape, and improve services, programs, and policies. Family leaders are families and caregivers who have received services at Holland Bloorview, and have lived experiences of paediatric disability. Family leaders’ roles include being a mentor to other families, an advisor to committees and working groups, and faculty who co-teach workshops to students and other families.
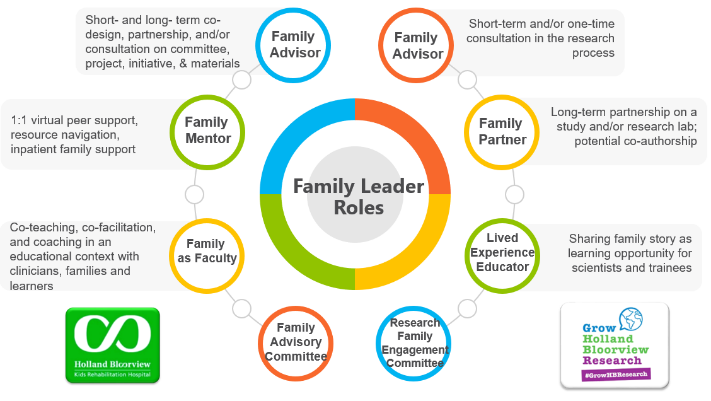
Family Leader Roles at Holland Bloorview. Photo provided with permission by Holland Bloorview Kids Rehabilitation Hospital.
The ENFit™ Working Group is an example of a successful implementation co-design process within Holland Bloorview. The ENFit™ Working Group is an interprofessional team working on the adoption of a new type of connection on products used for enteral feeding [feeding directly through the stomach or intestine via a tube]. By introducing the ENFit™ system, a best practice safety standard, the working group plans to reduce the risk of disconnecting the feeding tube from other medical tubes, and thus decrease harm to children and youth who require enteral feeding.
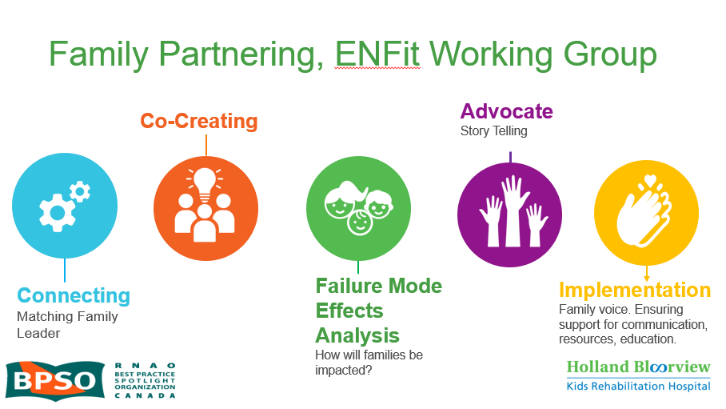
Family Partnering with the EnFit Working Group. Photo provided with permission by Holland Bloorview Kids Rehabilitation Hospital.
The working group invited a family member and leader whose son had received services at Holland Bloorview. This family member had significant lived experience with enteral feeding management, enteral medication administration, and other complexities associated with enteral products. During the meetings, great attention was given to the potential impacts on persons and families. The group engaged the family member by:
- co-creating the implementation plan
- involving them in a failure mode affects analysis, which highlighted the impact of the feeding tube supplies on transitions to home, school, and other care settings
- working with the family member to advocate for safe transitions within the provincial pediatric system, which led to the development of the Ontario Pediatric ENFit™ Group
To learn more about Holland Bloorview’s experience in partnering with families in a co-design process, watch their 38-minute webinar: The Power of Family Partnerships.

