BEST PRACTICE
Based on evidence such as best practice guidelines, quality indicators, decision-making algorithms, or systematic reviews
GAP
CURRENT PRACTICE
Existing practices, policies, health outcomes, attitudes, knowledge, skills within your organization/setting
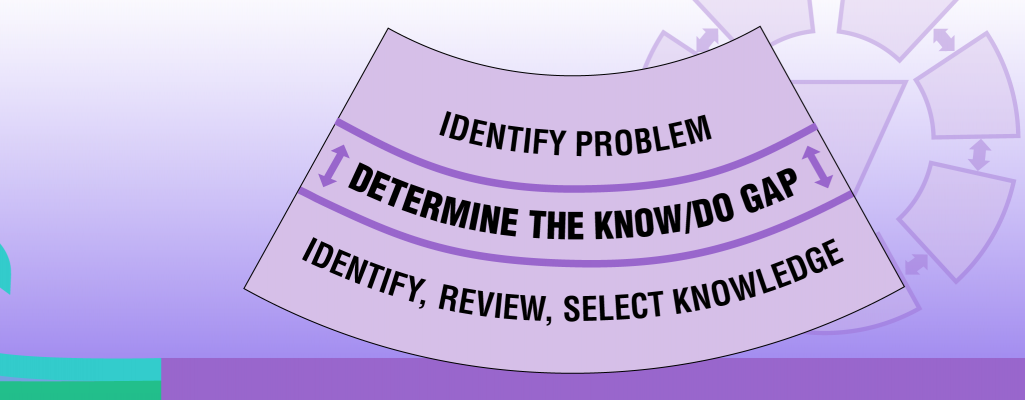
Once you and your team identified a problem or issue, you can determine the knowledge-to-practice gap. Here are some questions to help you identify this gap:
- What are the gaps between the best practice and current practice for the identified problem?
- In which contexts and to what extent do these gaps exist?
- Consider again, who may gain and who may lose if a particular gap is prioritized?
- Consider the potential for bias depending on who is defining the problem (e.g., a CEO and a nurse may identify different problems to prioritize)
SOURCE: Knowledge Translation Canada, 2020.
How do you assess the knowledge-to-practice gap and understand the size and nature of the gap?
- Use a systematic process for determining the size and nature of the gap. A gap (or opportunity) analysis allows for a detailed approach that uncovers multiple aspects of health-care delivery that may need to change such as attitudes, knowledge, skills, behaviours, practices, or policies. Conducting a gap analysis creates an opportunity to change practice and create excellence in care outcomes through the implementation of evidence.
- Use data, like survey results, informant interviews, chart audits, or evaluation results, to help determine the size and nature of the gap. Results from your gap analysis can also help you identify resource needs and pinpoint interventions (Golden et al., 2017).
- A gap (or opportunity) analysis may also help determine strengths, areas where best practices are partially implemented—which would be good places to start—and facilitators and barriers to implementation.
- When determining the knowledge-to-practice gap, engage multiple stakeholders and encourage “dynamic dialogue” and candid discussions. This improves engagement, supports creative solutions and helps unite a team in improving care.
SOURCES: Golden et al., 2017; Holmes et al., 2018; Kitson & Straus, 2013; RNAO, 2012.
Remember: Stakeholders may offer different knowledge sources and bring unique perspectives.
Consider all aspects and strive to reach a consensus before proceeding!
Prioritizing which knowledge-to-practice gap to address
Sometimes, you and your change team may identify multiple gaps that you want to address in a problem area. It can be helpful to determine prioritized areas of focus with input and feedback from other stakeholders, like the staff. To support decision-making regarding priority areas, the following questions can be helpful to discuss as a team. The questions are also available as a downloadable worksheet (see below to open).
- Is this gap an area of clinical concern?
- Does evidence (e.g., guidelines, systematic reviews, etc.) exist to address this gap?
- Are baseline data available to indicate current outcomes?
- Is there sufficient interest from key stakeholders to support work on this gap?
- Does addressing this gap have the support of your senior leadership team?
- Does addressing this gap align with other local, regional, or national activities?
- Would doing something be feasible, practical, and/or desirable?
SOURCE: Adapted from Kitson & Straus, 2013.
