
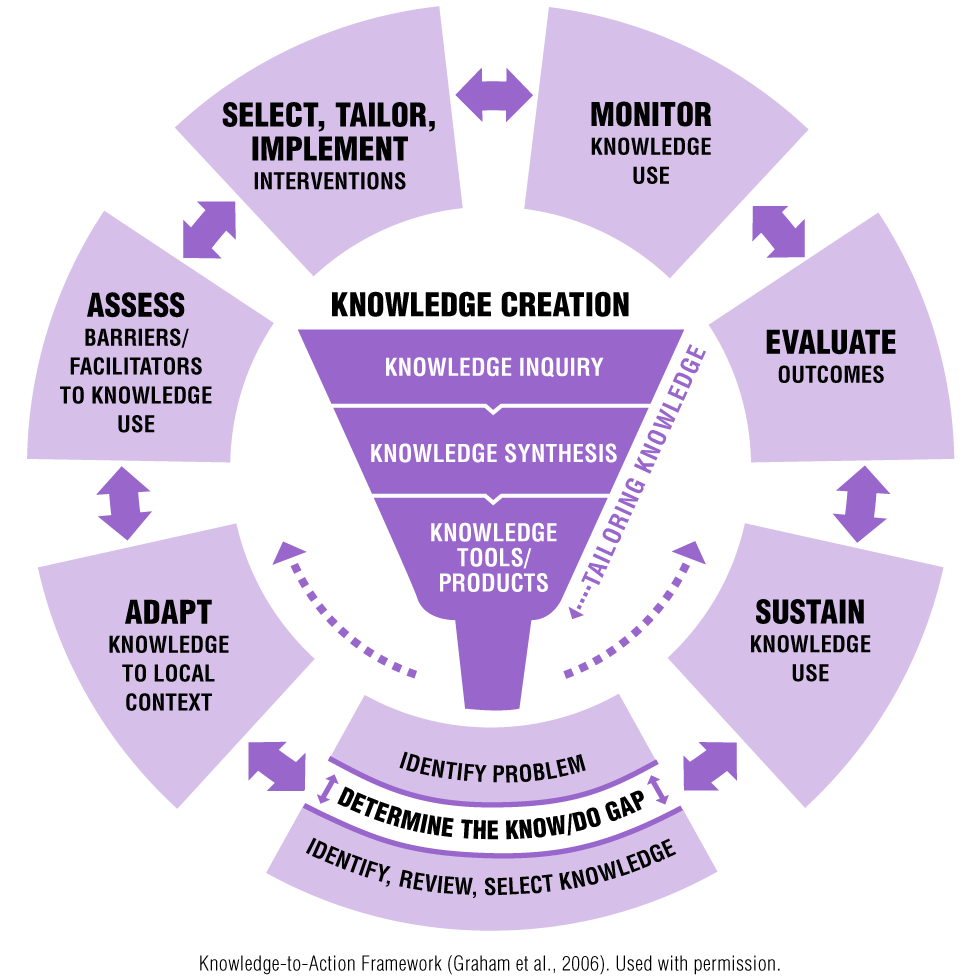
Using the KTA Framework, let’s look at how it can be applied to the implementation of Home Health Monitoring (HHM) for seniors who have an obstructive pulmonary disease (Lee & Ho, 2019).
|
Image
 |
Scenario The promise of Home Health Monitoring (HHM) for Chronic Obstructive Pulmonary Disease (COPD) is to: improve self-management by the person; reduce health-care system expenses; and establish potential use of data algorithms to predict episodes of exacerbation. The KTA Framework can be applied to guide HHM uptake so that enough skills and resources are harnessed to transfer knowledge across the various research and decision-making cultures within the organization.
|
In the table below, all of the KTA Framework Action Cycle phases are listed. The right-hand column illustrates how each action cycle phase can be applied to the implementation of HHM for seniors who have COPD (Lee & Ho, 2019).
| KTA Framework Action Cycle Phase | Applying the Action Cycle phases of the KTA Framework |
|---|---|
| Identify the problem |
|
| Adapt knowledge to local context |
|
| Assess barriers and facilitators |
|
| Select, tailor, and implement interventions |
|
| Monitor knowledge use |
|
| Evaluate outcomes |
|
| Sustain knowledge use |
|
Don’t worry if your implementation plans do not include all of the Action Cycle phases of the KTA Framework. To learn more about the framework and its phases, see Knowledge-to-Action Framework
