Through our advocacy work, ongoing consultations with the Ontario government, we are vigilant in our mission to enhance the nursing profession. Members are often among the first to learn of proposed changes to public policy and members often provide input in policy making decisions. RNAO regularly monitors and responds to issues relating to the nursing workforce, scope of practice, nursing culture and safety, education and regulation with evidence-based recommendations. RNAO continues to sound the alarm on the need to put more resources into primary care, home and community care to decrease the number of patients in hospital.
Take action
Hon. Pierre Poilievre, stop targeting transgender youth!
Canada is burning and our future is in peril! Act NOW, Premier Ford and Prime Minister Trudeau!
Current issues
Long-term care
Nursing policy
Opioid overdose crisis
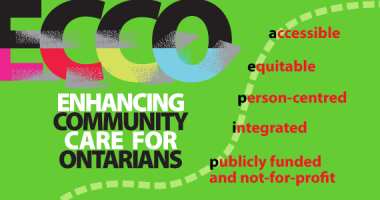
Our vision
Our vision is of an Ontario that creates the conditions for health and wellness for everyone by addressing the many determinants of health.
That means a system that is
Accessible
with interprofessional care teams anchored in the communities where people live, work and play.
Person-centred
where a person and their support system are viewed as a whole and empowered to be genuine partners for their own health.
Equitable
where deliberate efforts are made to decrease gaps in health outcomes, services and experiences.
Integrated
where care is coordinated so that transitions from sector to sector, service to service, are seamless.

Publicly funded and not-for-profit
so that it is efficient and sustainable and everyone, no matter their means, receives the care they require.
Upcoming events
Queen's Park on the Road (QPOR)
Queen's Park Day
Take Your MPP To Work
Find policy files
The RNAO policy library provides search for all our policy resources.